Chest MRI of a pregnant woman with COVID-19 pneumonia
- Authors: Vasilev Y.A.1,2, Bazhin A.V.3, Masri A.G.3, Vasileva Y.N.3,4, Panina O.Y.1, Sinitsyn V.E.1
-
Affiliations:
- Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Health Care Department
- City Clinical Oncological Hospital No. 1 of the Moscow Health Care Department
- City Polyclinic No. 3 of the Moscow Health Care Department
- Moscow State University of Medicine and Dentistry named after A.I. Evdokimov
- Issue: Vol 1, No 1 (2020)
- Pages: 61-68
- Section: Case reports
- URL: https://jdigitaldiagnostics.com/DD/article/view/46800
- DOI: https://doi.org/10.17816/DD46800
- ID: 46800
Cite item
Abstract
This paper presents a clinical case of a 39-year-old pregnant woman with respiratory signs of the novel coronavirus Covid-19 infection. Chest MRI showed bilateral lesions in basal segments. The PCR test was positive. A lung condition was assessed without loss of significant diagnostic information. Besides that, the absence of exposure to ionizing radiation allowed to avoid a high loading dose on the patient and the fetus. This case reveals potential opportunities of MRI in the diagnosis of pulmonary pathology without exposure to ionizing radiation, especially in patient risk groups (children, pregnant women, etc.).
Keywords
Full Text
INTRODUCTION
Diagnostic radiology of lung changes has become a part of the comprehensive medical evaluation of patients suspected with pneumonia caused by coronavirus disease 2019 (COVID-19). Since the method of choice is computed tomography (CT), visualization of the lungs in pregnant women raised significant difficulties. Notably, in Moscow, the average effective dose for a chest CT scan is 5.6 mSv [1]. Thus, a search for alternative non-ionizing methods led to performing magnetic resonance imaging (MRI) of the lungs.
CASE HISTORY
The patient was a 39-year-old woman at 26 weeks of gestation of her 4th pregnancy. The course of the pregnancy was satisfactory. She had no abortions and miscarriages. Previous pregnancies had no complications, which ended in birth of healthy children. Family history was unremarkable.
Epidemiological history: During her visit to the clinic, her husband and mother had manifestations of viral pneumonia. In July 2020, the patient came to the doctor with complaints of chest pain, body temperature up to 38.5°C, headache, and increased fatigue.
Physical examination: During auscultation, diminished vesicular breath sounds were heard, and crackles and wheezes were absent. Blood oxygen saturation based on pulse oximetry was 95%. During her visit, results of laboratory tests were unavailable. The result of the reverse-transcription polymerase chain reaction test for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 RT-PCR) was positive obtained after MRI.
Given the epidemiological history and clinical manifestations suspicious for COVID-19 infection, imaging examination of chest organs is necessary to clarify the etiology of the disease. To avoid adverse effects due to exposure of the pregnant woman and the fetus to large radiation doses, chest MRI was performed. Personal protective equipment was used to ensure safety–surgical masks without ferromagnetic components–during the entire stay in the radiology department.
Initially, T2-weighted images (T2WI) were obtained in three planes using a single-shot fast spin echo (SSFSE) with the following parameters: repetition time (TR), 1300 ms; echo time (TE), 80 ms; flip angle, 90°; field of view (FOV), 450–450 mm; matrix, 512 × 512; slice thickness, 6 mm; spacing between slices, 6 mm; number of averages, 0.6; k-space filling method, Cartesian. These images were applied for planning axial FSE T2WI.
T1-weighted imaging was performed by LAVA 3D and IDEAL 3D. For LAVA 3D, the scanning parameters were as follows: TR, 4 ms; TE, 2.2 ms and 1.1 ms; flip angle, 10°; FOV, 400–400 mm; matrix 512 × 512; slice thickness, 3 mm; spacing between slices, 1.5 mm; number of averages, 0.7 with WATER and FAT fractions, in-phase/out-phase. For IDEAL 3D, the scanning parameters were as follows: TR, 5.8 ms; TE, 2.5 ms; flip angle, 3°; FOV, 440–440 mm; matrix, 256 × 256; slice thickness, 10 mm; spacing between slices, 10 mm; number of averages 0.7 with WATER and FAT fractions, in-phase/out-phase.
Diffusion-weighted imaging was performed by EPI pulse sequence with these parameters: TR, 10000 ms; TE, 62.3 ms; flip angle, 89°; FOV, 400–400 mm; matrix, 128×140; slice thickness, 5 mm; spacing between slices, 5 mm; number of averages, 1; b-values, 50,800 s/mm2. The number of averages for SSFSE, LAVA-Flex, and EPI series was not higher than 1 to reduce blurring artifacts associated with the non-availability of respiratory gating. Free-breathing imaging study was conducted, a physical respiratory trigger was not used, but automatic synchronization was employed on the movement of the diaphragm to optimize the acquisition time.
The study was conducted in the supine position using abdominal and spinal radio frequency (RF) coils. The center of the abdominal coil was located in the middle of the sternum. To minimize dynamic artifacts associated with respiratory movements, the RF coil was fixed. The central laser beam was positioned at the mid-sternum.
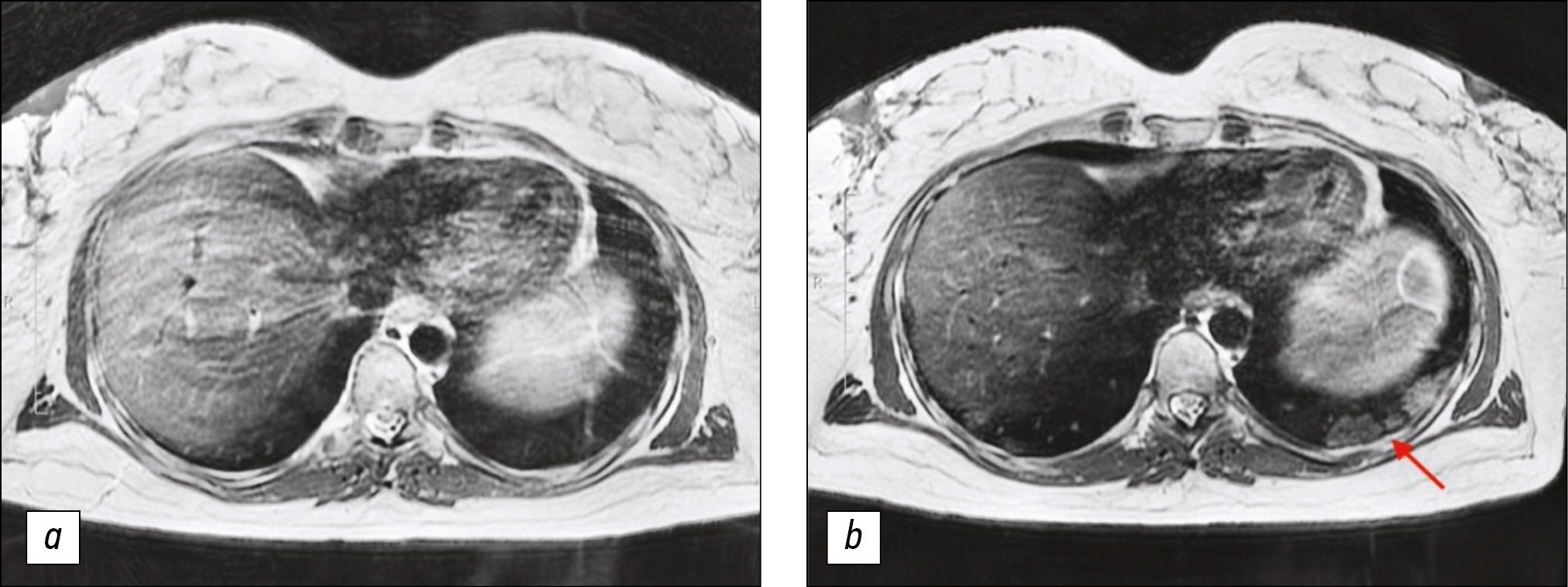
Lung MRI was performed 7 days later, because the condition did not improve during treatment, and dry, ineffective cough worsened. MRI performed that time revealed zones of infiltration (Figs. 1, 2) in the lower lobes of the lungs.
Figure 1. Chest magnetic resonance imaging, T2-weighted imaging single-shot fast spin echo: a) Primary examination, b) magnetic resonance imaging 7 days later. In Fig. 1b, consolidation zones in lower lungs appeared as areas of hyperintense and isointense signals.
Figure 2. Chest magnetic resonance imaging, T2-weighted imaging single-shot fast spin echo: a) Primary examination, b) magnetic resonance imaging 7 days later. In Fig. 2b, consolidation zones in the lower right lung appeared as areas of hyperintense signal.
DISCUSSION
In the present case, the diagnosis of SARS-CoV-2 infection was based on the epidemiological history, clinical manifestations, laboratory test results, chest CT findings, and a positive SARS-CoV-2 RT-PCR test result. All these methods are both useful and limited, as PCR test has a false-negative rate of at least 30%. Therefore, the diagnostic process should be complex [2]. The use of chest CT for COVID-19 screening is justified in patients with clinical and epidemiological suspicions, especially in cases with negative SARS-CoV-2 RT-PCR results [3].
The current pandemic has highlighted the importance of CT in the diagnosis and monitoring of COVID-19 pneumonia, as it is a more sensitive and effective method than X-ray. In addition, chest CT, including in pregnant women, contributes to early detection, severity assessment, and monitoring of treatment effects to patients with or without confirmation of SARS-CoV-2 [4–5]. CT is associated with high patient radiation exposure. If a dynamic observation is required, the radiation load is increased accordingly [1].
This report presents a unique case of performing MRI of the lungs in a pregnant woman with COVID-19 pneumonia. Moreover, the case demonstrates the dynamic development of the disease according to MRI data. Notably, this is not the first case of performing chest MRI in pregnant women [6–11]. Kapdagli et al. reported on the detection of chondrosarcoma of the right lung by MRI in a 23-year-old pregnant woman. The tumor size was 18×16×17.5 cm3, and it originated from the ribs [10]. Said et al. also described a rare case of primary lung liposarcoma diagnosed by MRI in a 28-year-old pregnant woman who complained of shortness of breath [11]. However, literature data on imaging of pregnant women with pneumonia caused by coronavirus infection were not available at the time of this writing. In this clinical case, the limitation was the inability to compare MRI and CT images. At present, no study has investigated MRI semiotics of COVID-19 pneumonia.
Currently, new pulse sequences, software, and modern technical equipment allow assessment of a lung condition using MRI [12]. Lung visualization is technically difficult due to the low density of the hydrogen protons in the lung parenchyma, as well as the rapid signal decay. However, pathological changes leading to tissue enlargement (“plus-tissue”), such as nodules, infiltrations, mucus, or pleural effusion, are easily detected with high diagnostic accuracy [14]. Although chest CT is more informative than MRI for detecting fine morphological structures, nowadays, MRI offers an increasing range of functional imaging techniques that surpass CT capabilities–perfusion, measurement of ventilation, and respiratory mechanics. Without a risk of exposing patients to ionizing radiation, repeated MRI examinations allow assessment of the disease course and quantitative monitoring of therapeutic response, providing a level of functional details that cannot be obtained with any other imaging method [15, 16].
The data presented herein can be useful when performing MRI of other body parts, in particular MRI of the breast, thoracic spine, and abdominal cavity. For example, abdominal MRI can detect findings in the lower chest [8]. Identified changes can be overlooked or misinterpreted because of their location outside the main focus area of the study, as well as unawareness of how pathological changes in the chest organs look on MRI scans.
CONCLUSION
MRI can be used to detect changes in the lung in pregnant women with suspected COVID-19 pneumonia. Given its certain advantages, MRI of the lungs can be considered a method of choice in cases where dynamic monitoring is required. With the continuous improvement in software of scanners, chest MRI is a prospective direction for the development of diagnostic radiology in detecting pulmonary pathology.
ADDITIONAL INFO
Funding. The publication had no sponsorship.
Conflict of interest. The authors declare no conflict of interest regarding this publication.
Authors contribution. All authors made a significant contribution to the search and analysis work and preparation of the article, read and approved the final version before publication.
Consent for publication. Written consent was obtained from the patient for publication of relevant medical information and all of accompanying images within the manuscript.
About the authors
Yuriy A. Vasilev
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Health Care Department; City Clinical Oncological Hospital No. 1 of the Moscow Health Care Department
Author for correspondence.
Email: dr.vasilev@me.com
ORCID iD: 0000-0002-0208-5218
SPIN-code: 4458-5608
Ph.D
Russian Federation, MoscowAlexander V. Bazhin
City Polyclinic No. 3 of the Moscow Health Care Department
Email: avbazhin@yandex.ru
ORCID iD: 0000-0003-3198-1334
SPIN-code: 6122-5786
Ph.D
Russian Federation, MoscowAmir G. Masri
City Polyclinic No. 3 of the Moscow Health Care Department
Email: amir.masri6@gmail.com
ORCID iD: 0000-0001-6294-1285
SPIN-code: 5357-1487
Russian Federation, Moscow
Yulia N. Vasileva
City Polyclinic No. 3 of the Moscow Health Care Department; Moscow State University of Medicine and Dentistry named after A.I. Evdokimov
Email: drugya@yandex.ru
ORCID iD: 0000-0003-4955-2749
SPIN-code: 9777-2067
Ph.D
Russian Federation, MoscowOlga Yu. Panina
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Health Care Department
Email: olgayurpanina@gmail.com
ORCID iD: 0000-0002-8684-775X
SPIN-code: 5504-8136
Junior Scientist Researcher
Russian Federation, MoscowValentin E. Sinitsyn
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Health Care Department
Email: v.sinitsyn@npcmr.ru
ORCID iD: 0000-0002-5649-2193
Professor
Russian Federation, MoscowReferences
- Morozov SP, Soldatov IV, Lantuh ZA, et al. Characteristic of radiation exposure of patients in medical centers of Moscow [Internet]. (In Russ). Available from: https://tele-med.ai/documents/482/harakteristika_dozovoj_nagruzki_na_pacientov_v_medicinskih_organizaciyah_g_moskvy_1.pdf
- Rajewska A, Mikołajek-bedner W, Lebdowicz-knul J, et al. COVID-19 and pregnancy – where are we now ? A review. J Perinat Med. 2020;48(5):428–434. doi: 10.1515/jpm-2020-0132
- Fang Y, Zhang H, Xie J, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296(2):E115–E117. doi: 10.1148/radiol.2020200432
- Liu H, Liu F, Li J, et al. Clinical and CT imaging features of the COVID-19 pneumonia: Focus on pregnant women and children. J Infect. 2020;80(5):e7–e13. doi: 10.1016/j.jinf.2020.03.007
- Gong XM, Song L, Li H, et al. CT characteristics and diagnostic value of COVID-19 in pregnancy. PLoS One. 2020;15(7):e0235134. doi: 10.1371/journal.pone.0235134
- Vremennye metodicheskie rekomendatsii. Profilaktika, diagnostika i lechenie novoi koronavirusnoi infektsii (COVID-19). Versiya 8 (utv. Ministerstvom zdravookhraneniya RF 3 sentyabrya 2020). (In Russ). Available from: https://base.garant.ru/74596434/
- Torkian P, Rajebi H, Zamani T, et al. Magnetic resonance imaging features of coronavirus disease 2019 (COVID-19) pneumonia: The first preliminary case series. Clin Imaging. 2021;69:261–265. doi: 10.1016/j.clinimag.2020.09.002
- Ates OF, Taydas O, Dheir H. Thorax magnetic resonance imaging findings in patients with Coronavirus Disease (COVID-19). Acad Radiol. 2020;27(10):1373–1378. doi: 10.1016/j.acra.2020.08.009
- Luchevaya diagnostika koronavirusnoi bolezni (COVID-19): magnitno-rezonansnaya tomografiya. Preprint. Seriya “Luchshie praktiki luchevoi i instrumental’noi diagnostiki”: Gosudarstvennoe byudzhetnoe uchrezhdenie zdravookhraneniya goroda Moskvy “Nauchno-prakticheskii klinicheskii tsentr diagnostiki i telemeditsinskikh tekhnologii Departamenta zdravookhraneniya goroda Moskvy” [Internet]. (In Russ). Available from: https://tele-med.ai/biblioteka-dokumentov/luchevaya-diagnostika-covid-19-mri
- Schloß M, Heckrodt J, Schneider C, et al. Magnetic resonance imaging of the lung as an alternative for a pregnant woman with pulmonary tuberculosis. J Radiol Case Rep. 2015;9(5):7–13. doi: 10.3941/jrcr.v9i5.2256
- Holzmann K, Kropfmüller R, Schinko H, et al. Lung cancer in pregnancy. Wien Klin Wochenschr. 2015;127(15-16):639–644. doi: 10.1007/s00508-015-0726-6
- Bin Saeedan M, Alabdulkarim FM, Aloufi FF, et al. Check the chest: review of chest findings on abdominal MRI. Clin Imaging. 2020;59(1):68–77. doi: 10.1016/j.clinimag.2019.10.005
- Oto A, Ernst R, Jesse MK, et al. Magnetic resonance imaging of the chest, abdomen, and pelvis in the evaluation of pregnant patients with neoplasms. Am J Perinatol. 2007;24(4):243–250. doi: 10.1055/s-2007-973444
- Kapdagli M, Erus S, Tanju S, Dilege S. Extensive chest wall resection, reconstruction and right pneumonectomy in a 24-week pregnant patient. Lung Cancer. 2018;(122):7–9. doi: 10.1016/j.lungcan.2018.05.005
- Said M, Migaw H, Hafsa C, et al. Imaging features of primary pulmonary liposarcoma. Australas Radiol. 2003;47(3):313–317. doi: 10.1046/j.1440-1673.2003.01198.x
- Alì M, Monti CB, Secchi F, et al. Fast thoracic MRI as an alternative to chest x-ray: A retrospective evaluation of 287 patients. Clin Imaging. 2020;60(2):244–248. doi: 10.1016/j.clinimag.2019.12.016
- Romei C, Turturici L, Tavanti L, et al. The use of chest magnetic resonance imaging in interstitial lung disease: A systematic review. Eur Respir Rev. 2018;27(150):180062. doi: 10.1183/16000617.0062-2018
- Wielpütz M, Kauczor HU. MRI of the lung: State of the art. Diagnostic Interv Radiol. 2012;18(4):344–353. doi: 10.4261/1305-3825.DIR.5365-11.0
- Zeng J, Liu Z, Shen G, et al. MRI evaluation of pulmonary lesions and lung tissue changes induced by tuberculosis. Int J Infect Dis. 2019;82:138–146. doi: 10.1016/j.ijid.2019.03.004
Supplementary files