Астроцитома головки зрительного нерва
- Авторы: Гольцман Е.В.1, Потемкин В.В.2,1, Астахов Ю.С.2, Марченко О.А.1, Антонов В.А.2, Кельина А.Е.3
-
Учреждения:
- СПбГУЗ «Городская многопрофильная больница № 2»
- ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. академика И.П. Павлова» Минздрава России
- ГАУЗ АО ФГБОУ ВО «Северо-Западный государственный медицинский университет им. И.И. Мечникова» Минздрава России
- Выпуск: Том 12, № 2 (2019)
- Страницы: 73-79
- Раздел: Клинические случаи
- Статья получена: 01.04.2019
- Статья одобрена: 06.05.2019
- Статья опубликована: 12.06.2019
- URL: https://journals.eco-vector.com/ov/article/view/11574
- DOI: https://doi.org/10.17816/OV2019273-79
- ID: 11574
Цитировать
Аннотация
В рамках данной статьи представлен клинический случай астроцитомы головки зрительного нерва у пациента с нейрофиброматозом 1-го типа. Особенностью случая является сложность дифференциальной диагностики с беспигментной меланомой хориоидеи.
Ключевые слова
Полный текст
В январе 2019 г. на отделение офтальмологии № 5 ГМПБ № 2 обратился пациент 72 лет с жалобами на постепенное безболезненное снижение зрения левого глаза в течение 10 лет. Впервые незначительное ухудшение зрения левого глаза отметил ещё в 2009 г. В медицинском учреждение по месту жительства был выставлен диагноз кисты сетчатки и рекомендовано наблюдение. В течение последующих 9 лет пациент регулярно посещал офтальмолога один раз в год — наблюдалась постепенная отрицательная динамика по остроте зрения. В 2018 г. произошло стремительное ухудшение зрения левого глаза, в связи с чем пациент обратился в другое офтальмологическое учреждение, где был поставлен диагноз новообразования хориоидеи левого глаза, вторичной отслойки сетчатки и рекомендована энуклеация.
Важный аспект анамнеза заболевания заключался в наличии нейрофиброматоза 1-го типа, который был установлен, когда пациенту было 43 года. На момент осмотра имелись следующие проявления заболевания: множественные кофейные пятна на коже головы, а также на теле различного размера, некоторые из которых достигали 1,5 см, а также множественные подкожные нейрофибромы (рис. 1).
Рис. 1. Пятна цвета кофе с молоком на коже рук и головы и подкожные нейрофибромы при нейрофиброматозе 1-го типа
Fig. 1. Coffee with milk spots (arms and head) and dermal neurofibroma in patient with neurofibromatosis type 1
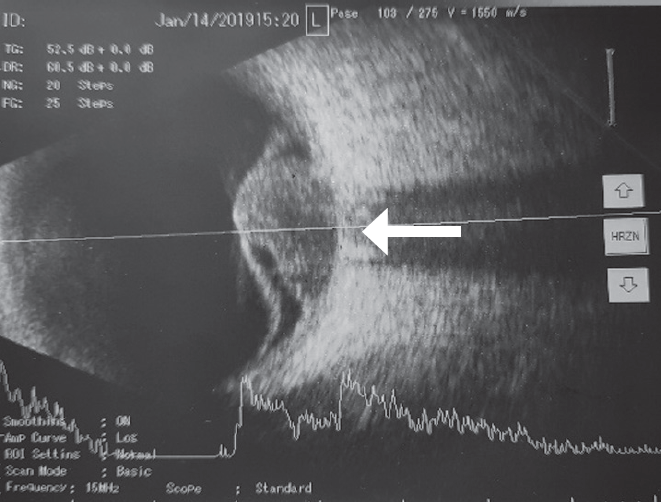
Данные офтальмологического обследования: визометрия правого глаза — 0,8 н/к, левого глаза — движение руки у лица; тонометрия — 18/17 мм рт. ст. При биомикроскопии передний отрезок обоих глаз — без особенностей. Особое внимание было уделено поиску узелков Лиша в радужной оболочке, которых мы не обнаружили. Офтальмоскопия: OD — очаговой патологии не выявлено; OS — над диском зрительного нерва проминирующее новообразование розовато-оранжевого цвета, многоузловое, с чёткими контурами, прикрывающее диск зрительного нерва, у основания которого в нижних отделах визуализируется отслойка сетчатки (рис. 2). По данным ультразвукового В-сканирования у диска зрительного нерва определялось проминирующее образование грибовидной формы (высота — до 6,7 мм, диаметр — до 13,0 мм), средней эхогенности, неоднородной плотности, у основания которого, в нижних отделах, отслоена сетчатка (рис. 3). Данные магнитно-резонансной томографии орбит также подтверждали наличие новообразования левого глаза (рис. 4).
Рис. 2. Астроцитома головки зрительного нерва. Чёрными стрелками указаны выступающие части опухоли
Fig. 2. Astrocytoma of the optic nerve head. Black arrows demonstrate a lobular structure of the tumor
Рис. 3. Ультразвуковое В-сканирование левого глаза. Опухоль располагается непосредственно над зрительным нервом (белая стрелка), вызывая вторичную отслойку сетчатки
Fig. 3. B-scan ultrasound of left eye. Tumor grows from optic nerve (white arrow) causing secondary retinal detachment
Рис. 4. Магнитно-резонансная томография орбит. Видна внутриглазная опухоль в проекции зрительного нерва
Fig. 4. MRI of orbits. Intaocular tumor over the optic nerve
Описанный клинический случай вызывает интерес ввиду сложности дифференциальной диагностики между беспигментной меланомой хориоидеи и астроцитомой головки зрительного нерва. Грибовидная форма новообразования, вторичная отслойка сетчатки, степень проминенции в стекловидное тело, а также возраст пациента говорили в пользу беспигментной меланомы. Однако нейрофиброматоз 1-го типа в анамнезе у пациента, десятилетний анамнез наличия внутриглазного новообразования («кисты сетчатки»), многодольчатость строения, а также локализация новообразования непосредственно над диском зрительного нерва позволили предположить диагноз астроцитомы.
На рис. 5 представлена типичная астроцитома головки зрительного нерва, а на рис. 6 — беспигментная меланома юкстапапиллярной локализации. Наиболее характерными симптомами астроцитомы являются чёткие контуры, жёлтый, оранжевый, розовый цвета или их сочетание, многодольчатость в различных её проявлениях (зачастую в виде тутовой ягоды). Астроцитома сетчатки и головки зрительного нерва чаще всего встречается в рамках симптомокомплекса туберозного склероза, но может развиваться и на фоне нейрофиброматоза 1-го типа или без какого-либо фонового заболевания [1, 2, 9, 14]. Типичная астроцитома головки зрительного нерва часто имеет вид тутовой ягоды за счёт множественных узлов кальцификации. Однако не стоит забывать, что встречаются астроцитомы без участков кальцификации [1, 2]. Обе опухоли могут сопровождаться вторичной отслойкой сетчатки [2, 9]. Беспигментная меланома юкстапапиллярной локализации может распространяться на головку зрительного нерва, но никогда не исходит непосредственно из неё, как в представленном клиническом случае. Помимо типичной лентикулярной формы, меланома может принимать грибовидную форму (или иметь вид запонки) за счёт прорастания мембраны Бруха и ущемления верхушки новообразования в сформированном дефекте [1]. Нередко меланома хориоидеи приобретает двугорбый вид, который свидетельствует о наличии двух эпицентров роста, обычно при развитии из предшествующего невуса. Однако мы никогда не наблюдали многодольчатого строения меланомы хориоидеи. При В-сканировании для меланомы сосудистой оболочки характерны эхогенность ниже средней, иногда наличие акустических полостей, а также симптом экскавации хориоидеи [1, 2]. При циркулярном росте вокруг диска зрительного нерва меланома хотя и может прорастать его, но проминенция опухоли над ним не является максимальной.
Рис. 5. Астроцитома головки зрительного нерва у мужчины 56 лет. Узлы кальцификации показаны чёрными стрелками, они лучше визуализируются в бескрасном свете
Fig. 5. Astrocytoma of the optic nerve head in 56 year old man. Nodules of calcification are marked with black arrows, better visualization in red-free light
Рис. 6. Беспигментная меланома хориоидеи юкстапапиллярной локализации с зоной прорастания мембраны Бруха (чёрные стрелки). При В-сканировании видна глубокая экскавация хориоидеи (белая стрелка)
Fig. 6. Amelanotic juxtapapillary choroidal melanoma penetrating Bruch’s membrane (black arrows). B-scan demonstrates deep choroidal excavation (white arrow)
Авторы статьи крайне редко прибегают к биопсии внутриглазных новообразований, так как диагноз в подавляющем большинстве случаев может быть поставлен на основании клинической картины. Но, учитывая описанные выше сложности в постановке окончательного диагноза, от которого зависела не только дальнейшая тактика в отношении сохранения глаза, но и прогноз для жизни, было принято решение о проведении тонкоигольной аспирационной биопсии. Предварительно пациенту была выполнена барьерная лазерная коагуляция сетчатки вокруг новообразования. Затем под внутривенной анестезией была проведена тонкоигольная аспирационная биопсия 27 G под прямым визуальным контролем без витрэктомии с последующим цитологическим исследованием материала. Результат цитологии: фрагменты опухолевой ткани, состоящие из мелких, относительно монотонных, округло-овальных и вытянутых клеток с короткими, невыраженными отростками цитоплазмы, отсутствием пигмента и плотным расположением в пласте. Митозов и некрозов не выявлено. Данных за меланому нет. Новообразование доброкачественное, предположительно из оболочек нерва.
Таким образом, благодаря тонкоигольной аспирационной биопсии был поставлен окончательный диагноз: «Астроцитома головки зрительного нерва». Энуклеация в данном случае не показана. Принимая во внимание, что острота зрения на момент обращения уже составляла движение руки у лица с неправильной проекцией света, отсутствовали офтальмогипертензия и болевой синдром, отслойка сетчатки была отграничена лазер-коагулянтами, а анамнез заболевания указывал на медленный рост в течение последних 10 лет, было решено воздержаться от попыток какого-либо лучевого или лазерного лечения в пользу динамического наблюдения с контролем результатов В-сканирования 1 раз в 3 месяца.
Под термином «внутриглазная астроцитома» подразумевают низкодифференцированное новообразование, берущее начало из сетчатки или из зрительного нерва до lamina cribrosa (головка зрительного нерва). Астроцитомы этой локализации принципиально отличаются от астроцитарных гамартом и реактивного астроцитоза (так называемого массивного глиоза) прогрессивным автономным ростом [9]. В клинической практике различия между астроцитомами, гамартомами и реактивным астроцитозом очень размытые. Внутриглазные астроцитомы представляют собой доброкачественные новообразования, однако могут приводить к потере зрения [9].
Возраст пациентов с впервые выявленной внутриглазной астроцитомой варьирует от 1 месяца до 45 лет. Размеры астроцитомы также могут значительно различаться: описаны опухоли размером всего в несколько миллиметров и опухоли, заполняющие всё глазное яблоко. Внутриглазная астроцитома может быть односторонней или двусторонней, одиночной или множественной, кальцифицированной или некальцифицированной. Нередко астроцитома может симулировать ретинобластому у детей, а у взрослых — беспигментную меланому или метастаз хориоидеи [4, 7, 8, 13]. Источником внутриглазных астроцитом чаще служит сетчатка. По данным одного из исследований, среди 1278 внутриглазных астроцитом лишь 1,6 % локализовались в головке зрительного нерва [10].
Наличие астроцитом сетчатки и зрительного нерва часто сопряжено с наличием туберозного склероза, реже — нейрофиброматоза. Так, по данным одного исследования, из 42 внутриглазных астроцитом 57 % были ассоциированы с туберозным склерозом, 14 % — с нейрофиброматозом и 29 % были спорадическими [12].
Нейрофиброматоз 1-го типа (болезнь Реклингхаузена) — наиболее часто встречающееся заболевание из группы факоматозов. Впервые заболевание было описано немецким врачом Friedrich Daniel von Recklinghausen в 1882 г. Оно характеризуется широким диапазоном и вариабельностью клинических проявлений с вовлечением различных органов и систем [10].
Основу диагностики нейрофиброматоза составляет обнаружение диагностических критериев, определённых Национальным институтом здоровья США в 1987 г. [5]. При наличии у пациента по крайней мере двух из перечисленных ниже признаков диагноз нейрофиброматоза не вызывает сомнений [5]:
- не менее 5 пятен цвета кофе с молоком диаметром более 5 мм у детей препубертатного возраста и не менее шести таких пятен диаметром более 15 мм в постпубертатном периоде;
- две и более нейрофибромы любого типа или одна плексиформная нейрофиброма;
- множественные мелкие пигментные пятна типа веснушек, локализованные в крупных кожных складках (подмышечных или паховых);
- глиома зрительного нерва;
- два и более узелка Лиша на радужной оболочке;
- костные аномалии (истончение кортикального слоя трубчатых костей, часто приводящее к формированию ложных суставов);
- наличие у родственников первой степени родства нейрофиброматоза 1-го типа по вышеуказанным критериям [12].
Нейрофиброматоз имеет множество офтальмологических проявлений. Наиболее часто встречаются узелки Лиша [11, 12]. Развитие плексиформной нейрофибромы в толще века может стать причиной S-образной глазной щели. Нередко нейрофиброматоз сопровождается развитием глиомы зрительного нерва. По данным литературы, последние отмечаются примерно у 15–25 % пациентов с нейрофиброматозом 1-го типа [6].
Как правило, астроцитомы требуют лишь наблюдения. Однако в случае массивной экссудации и отслойки сетчатки могут быть выполнены лазерная коагуляция сетчатки, криотерапия, фотодинамическая терапия или брахитерапия [1, 6].
Таким образом, диагностика астроцитом сетчатки и головки зрительного нерва не всегда очевидна ввиду разнообразия клинических проявлений. Одна из самых сложных задач состоит в дифференциальной диагностике с беспигментной меланомой и метастазом хориоидеи, ведь от этого зависят и дальнейшая тактика, и прогноз для жизни пациента.
Об авторах
Елена Владимировна Гольцман
СПбГУЗ «Городская многопрофильная больница № 2»
Email: ageeva_elena@inbox.ru
врач-офтальмолог
Россия, Санкт-ПетербургВиталий Витальевич Потемкин
ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. академика И.П. Павлова» Минздрава России; СПбГУЗ «Городская многопрофильная больница № 2»
Автор, ответственный за переписку.
Email: potem@inbox.ru
канд. мед. наук, доцент кафедры офтальмологии; врач-офтальмолог
Россия, Санкт-ПетербургЮрий Сергеевич Астахов
ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. академика И.П. Павлова» Минздрава России
Email: astakhov73@mail.ru
д-р мед. наук, профессор кафедры офтальмологии, кафедра офтальмологии
Россия, Санкт-ПетербургОльга Анатольевна Марченко
СПбГУЗ «Городская многопрофильная больница № 2»
Email: oamarchenko@yandex.ru
врач-офтальмолог
Россия, Санкт-ПетербургВладимир Александрович Антонов
ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. академика И.П. Павлова» Минздрава России
Email: antonov@alborada.fi
ординатор кафедры офтальмологии
Россия, Санкт-ПетербургАнастасия Евгеньевна Кельина
ГАУЗ АО ФГБОУ ВО «Северо-Западный государственный медицинский университет им. И.И. Мечникова» Минздрава России
Email: stokecity@bk.ru
студентка
Россия, Санкт-ПетербургСписок литературы
- Бровкина А.Ф. Офтальмоонкология. Руководство для врачей. – М.: Медицина, 2002. [Brovkina AF. Oftal’moonkologiya. Rukovodstvo dlya vrachey. Moscow: Meditsina; 2002.(In Russ.)]
- Бровкина А.Ф. Дифференциальная диагностика меланомы хориоидеи // Офтальмологические ведомости. – 2008. – Т 1. – № 4. – С. 68–76. [Brovkina AF. Differential diagnosis of choroidal melanoma. Oftal’mologicheskie vedomosti. 2008;1(4):68-76. (In Russ.)]
- Dutton JJ. Gliomas of the anterior visual pathway. Surv Ophthalmol. 1994;38(5):427-452. https://doi.org/10.1016/0039-6257(94)90173-2.
- DeBustroas S, Miller NR, Finkelstein D, et al. Bilateral astrocytic hamartomas of the optic nerve heads in retinitis pigmentosa. Retina. 1983;3(1):21-23.
- Stumpf DA, Alksne JF, Annegers F, et al. NIH consensus development conference: neurofibromatosis conference statement. Arch Neurol. 1988;45:575-578.
- Listernick R, Ferner RE, Liu GT, Gutmann DH. Optic pathway gliomas in neurofibromatosis-1: controversies and recommendations. Ann Neurol. 2007;61(3):189-198. https://doi.org/10.1002/ana.21107.
- Martyn LJ, Knox DL. Glial hamartoma of the retina in generalized neurofibromatosis, Von Recklinghausen’s disease. Br J Ophthalmol. 1972;56(6):487-491. https://doi.org/10.1136/bjo.56.6.487.
- Narayanan V. Tuberous sclerosis complex: genetics to pathogenesis. Pediatr Neurol. 2003;29(5):404-409. https://doi.org/10.1016/j.pediatrneurol.2003.09.002.
- Pusateri A, Margo CE. Intraocular astrocytoma and its differential diagnosis. Arch Pathol Lab Med. 2014;138(9):1250-1254. https://doi.org/10.5858/arpa.2013-0448-RS.
- Riccardi VM. Neurofibromatosis: past, present, and future. N Engl J Med. 1991;324(18):1283-1285. https://doi.org/10.1056/NEJM199105023241812.
- Recupero SM, Plateroti R, Abdolrahimzadeh S, et al. Lisch nodules in neurofibromatosis type 1: relationship to age and cutaneous neurofibromas. Annals of ophthalmology-glaucoma. 1996;28(3):178-183.
- Ragge NK, Falk RE, Cohen WE, Murphree AL. Images of Lisch nodules across the spectrum. Eye (Lond). 1993;7 (Pt 1):95-101. https://doi.org/10.1038/eye.1993.20.
- Shields JJ, Shields CL. Intraocular tumors: A text and atlas. Philadelphia, PA: WB Saunders Co; 1992.
- Ulbright TM, Fulling KH, Helveston EM. Astrocytic tumors of the retina. Differentiation of sporadic tumors from phakomatosis-associated tumors. Arch Pathol Lab Med. 1984;108(2): 160-163.
Дополнительные файлы