Treatment of pediatric patients with lower extremity deformities using software-assisted Ortho-SUV Frame: analysis of 213 cases
- 作者: Vilensky V.A.1, Pozdeev A.A.1, Zubairov T.F.1, Zakharyan E.A.1, Pozdeev A.P.2
-
隶属关系:
- The Turner Scientific and Research Institute for Children’s Orthopedics
- MD, PhD, professor, chief research associate of the department of bone pathology
- 期: 卷 4, 编号 4 (2016)
- 页面: 21-32
- 栏目: Articles
- ##submission.dateSubmitted##: 09.01.2017
- ##submission.dateAccepted##: 09.01.2017
- ##submission.datePublished##: 14.12.2016
- URL: https://journals.eco-vector.com/turner/article/view/5892
- DOI: https://doi.org/10.17816/PTORS4421-32
- ID: 5892
如何引用文章
详细
Aim. To retrospectively assess treatment outcomes of long bone deformities of the lower extremities accompanied by shortening in pediatric patients using a software-assisted Ortho-SUV Frame.
Materials and methods. The accuracy of deformity correction (AC), period of deformity correction (PDC), external fixation index (EFI), and number of complications in 213 patients were retrospectively analyzed.
Results. According to different parameters, AC of femur deformity correction (group 1) varied from 90% to 96%. The average length increase was 47 ± 12 mm. The average distraction duration was 38 ± 14 days. The average PDC was 8 ± 6 days for simple deformities (SDs), 14 ± 7 days for moderate deformities (MDs), and 23 ± 12 days for complex deformities (CDs). EFI was 26 ± 8 days/cm for SDs, 31 ± 6 days/cm for MDs, and 35 ± 12 days/cm for CDs. According to different parameters, AC of the lower leg deformity correction (group 2) varied from 89% to 95%. The average length increase was 52 ± 20 mm. The average distraction duration was 45 ± 18 days. PDC was 11 ± 5 days for SDs, 16 ± 9 days for MDs, and 27 ± 16 days for CDs. EFI was 32 ± 14 days/cm for SDs, 42 ± 12 days/cm for MDs, and 49 ± 8 days/cm for CDs. There were 48 (50.5%) complications in group I with the majority (71%) classified as Caton grade I and 29% as grade II. There were 62 (45%) complications in group 2, where 50% were Caton grade I and 50% were Caton grade II. There were no serious complications (Caton grade III) in either group that influenced the final functional results.
Conclusion: Use of a software-assisted Ortho-SUV Frame increased the efficiency of treatment of pediatric patients with long bone deformities because of the great accuracy of deformity correction.全文:
Introduction
Currently, transosseous osteosynthesis is the main treatment for complex, multi-component deformities of long bones that are accompanied by shortening in pediatric patients. The use of the Ilizarov frame is a traditional method that enables the surgeon to perform a deformity correction of any complexity while extending the bone segment [1-5]. However, a number of studies provide evidence that using the standard reference lines and angles (RLA) of the Ilizarov frame [3, 6-8] does not result in an accurate deformity correction: ranging from 0% in the correction of complex deformities to 79% in the correction of simple deformities [9, 10]. This is likely due to the fact that when using the Ilizarov frame, the position of the bone fragments is changed spatially by the unit assemblies; each unit assembly eliminates only one component of the deformity. Therefore, the elimination of a complex multi-component deformity requires their repeated replacement [2, 4, 11, 12].
The contemporary transosseous frames of the hexapod group use calculations made in computer navigation programs to propel the correction accuracy to a new level: ranging from 86% to 94% for complex multi-component multiplanar deformities[3, 10-14].
One of the frames in this group, the Ortho-SUV Frame, is the only Russian hexapod to date [15, 16]. The function and properties of this frame is based on the original kinematic platform. Studies have demonstrated that the Ortho-SUV Frame has superior repositioning opportunities [17] and fixation stability [18] over other hexapod frames. In fact, the Ortho-SUV Frame utilizes a flexible joint attachment that allows multiple assemblies and can be used with the external supports of virtually any transosseous frame [16]. Despite widespread clinical use, studies investigating its application remain limited to those demonstrating its efficiency in correcting femoral deformities in adults [12, 19]. There are no publications to date that have assessed the efficiency of this device for the correction of deformities of long bones in pediatric patients.
Aims: To investigate the accuracy and efficacy of the software-assisted Ortho-SUV Frame for the transosseous osteosynthesis of long bone deformities of lower extremities with shortening in pediatric patients through retrospective analysis of the surgical treatment outcomes using this method.
Materials and methods
The study included 213 pediatric patients with deformities of the long bones of the lower extremities due to various congenital malformations (105 cases), diseases of the musculoskeletal system (78 cases), and trauma (30 cases).
All patients were treated between 2011 and 2015 in the department No1 of the Federal State Budgetary Institution of the Turner Scientific and Research institute for Children’s Orthopedics. Each participant’s parent or guardian voluntarily signed informed consents for surgery and for participation in the study. The distribution of patients according to nosology is presented in the Table 1. The minimum age at the onset of treatment was 4 years, the maximum age was 17 years, and the average age was 12 years.
Table 1.Distribution of patients according to nosology
Diagnosis | Number of patients (segments surgically treated) | Diagnosis | Number of patients (segments surgically treated) |
Consequences of hematogenous osteomyelitis | 22 (26) | Multiple exostosis chondrodysplasia | 7 (10) |
Achondroplasia | 13 (23) | Oilier’s disease | 11 (14) |
Phosphate diabetes | 8 (14) | Consequence of Perthes disease | 2 (2) |
Fibrous dysplasia | 1 (1) | Blount disease | 11 (11) |
Cleveland-Evans syndrome | 1 (2) | Idiopathtic pseudarthrosis of femur | 1 (1) |
Consequences of juvenile epiphysiolysis | 1 (1) | Congenital malformation of tibia | 22 (22) |
Congenital femoral shortening | 20 (20) | Consequence of congenital pseudarthrosis of tibia | 36 (36) |
Congenital coxa vara | 9 (11) | Consequences of congenital hip dislocation | 4 (4) |
Congenital malformation of femur and tibia | 12 (18) | Post-traumatic tibial deformity | 9 (9) |
Congenital posteroexternal cnemoscoliosis | 2 (2) | Post-traumatic femoral pseudarthrosis | 1 (1) |
Post-traumatic femoral deformity | 16 (16) | Post-traumatic tibial pseudarthrosis | 2 (2) |
Post-traumatic deformity of femur and tibia | 2 (4) | Total | 213 (253) |
The main criteria for the selection of patients for this type of treatment were the following: the presence of a deformity with an associated shortening of the bone segment; cases in which it was impossible to achieve correction by applying external osteosynthesis (due to the presence of functioning zones of growth, the location of the deformity apex at the level of the joint space or beyond the segment, etc.); and patients with a follow-up period of at least 1 year.
Deformities with the apex at the diaphysis level were seen in 75 patients (87 segments); those at the metaphyseal level were seen in 109 patients (134 segments) and combined two-level deformities were noted in 29 patients (32 segments).
Femoral deformity correction was performed in 101 cases (94 patients, Group 1), and deformity correction of the tibial bone was performed in 152 cases (119 patients, Group 2).
Long bone deformities were classified according to the practical classification of long bone deformities [21], and the following deformities were included in the present study: 15 simple deformities (single-plane, one-component deformities that included 3 hips and 12 tibias), 118 moderate deformities (single-, two-, and three-plane, two- and three-component deformities that included 72 hips and 46 tibias), 120 complex deformities (two- and three-plane, multi-component deformities that included 26 hips and 94 tibias).
In most cases (195 patients), the application of the Ortho-SUV Frame was combined with that of the Ilizarov frame. During the first stage of the procedure, the extension was performed at the osteotomy level on the threaded rods of the Ilizarov frame. Once the desired extension was achieved, the Ortho-SUV frame assembly was mounted and its rings were connected at the osteotomy level. Subsequently, the threaded rods were removed, and the software program used the X-ray images to calculate the amount of correction required. After performing the radiographically confirmed deformity correction, the Ortho-SUV frame was replaced with the threaded rods of the Ilizarov frame to prevent any change in the position of the rings that had been achieved during the correction.
In 18 cases, the Ortho-SUV frame was mounted intraoperatively; in the early postoperative period, the extension and correction of the deformity was calculated by the computer program, and the deformity extension and correction was performed simultaneously.
Antero-posterior and lateral view panoramic radiographs of both lower limbs were taken pre-operatively and post-operatively for all patients.
The indices of the reference lines and angles (RLAs) were evaluated before the correction, after the correction, after the removal of the external fixation device (EFD), and in the follow-up period. The results were compared with normal values. For the treatment of the femoral deformities, the following RLAs were evaluated: the mechanical lateral proximal femoral angle (mLPrFA), the mechanical lateral distal femoral angle (mLDFA), the mechanical axis deviation (MAD), and the anatomical posterior distal femoral angle (aPDFA). For the treatment of tibial deformities, the following parameters were evaluated: the mechanical medial proximal angle of the tibia (mMPrAT), the mechanical lateral distal angle of the tibia (mLDAT), the MAD, the anatomical posterior proximal tibial angle (aPPTA), and the anatomical anterior distal tibial angle (aADTA). It should be noted that the MAD was evaluated only for those cases in which the deformity was a “single-segment” so correction of the adjacent segment was not required, and evaluation of the outcome was possible. Software programs BoneNinja (USA) and TraumaCad (Israel) were used for the construction and evaluation of the RLAs.
The value of the torsional component of the deformity was determined both clinically and by computed tomography.
The time of distraction (TD), the period of the deformity correction (PC), and the external fixation index (EFI) were also evaluated. Complications were evaluated according to the three grades established by the classification of J. Caton (1991) [21]: grade I implies mild complications that disappear at the end of extension, grade II implies moderate complications that require emergency surgery and do not impair the functional outcome of the treatment, and grade III implies serious complications that impair the functional outcome of the treatment.
Results
Group 1. During the femoral deformity correction, we obtained the results shown in Table 2. Thus, in the varus deformity correction, the average value of MAD was 3 ± 8 mm inwards, whereas in the valgus deformity correction was 1 ± 6 mm inwards; the change in the postoperative value of MAD compared with the preoperative value amounted to an average of 28 mm for the varus deformities and 37 mm for the valgus deformities. These results are consistent with the range of normal values. The MAD values exceeded the normal limits in only 9 out of 101 cases. Thus, the accuracy of the deformity correction of the MAD was 91%.
Table 2. The reference lines and angles in the femoral deformities correction
Indicator | Normal values | Before the treatment | After the treatment |
Frontal view | |||
Varus | |||
MAD, mm | 0–9.7 medially | 31 ± 12 medially | 3 ± 8 medially |
mLPrFA, ° | 85–95 | 108 ± 15 | 89 ± 6 |
mLDFA, ° | 85–90 | 97 ± 12 | 87 ± 5 |
Valgus | |||
MAD | 0–9.7 medially | 38 ± 18 laterally | 1 ± 6 laterally |
mLPrFA, ° | 85–90 | 74 ± 10 | 86 ± 8 |
mLDFA, ° | 86–92 | 82 ± 12 | 89 ± 6 |
Sagittal plane | |||
Recurvation | |||
aPDFA, ° | 73–84 | 92 ± 9 | 83 ± 11 |
Antecurvature | |||
aPDFA, ° | 73–84 | 65 ± 14 | 77 ± 9 |
Note: mLPrFA is the mechanical lateral proximal femoral angle; mLDFA is the mechanical lateral distal femoral angle; MAD is the mechanical axis deviation; aPDFA is the anatomical posterior distal femoral angle.
The magnitude of the angular correction of the femur in the frontal view averaged 22 ± 7º for the varus deformities, whereas it averaged 15 ± 11º for the valgus deformities. The correction accuracy of the mLPrFA and mLDFA for the varus deformities was 96%, and for the valgus deformities it was 93%.
The magnitude of the angular correction of the femur in the sagittal plane averaged 11 ± 9º for the antecurvature deformities, whereas it averaged 8 ± 9º (ranging from 3 to 42º) for recurvature deformities. The correction accuracy for the antecurvature deformities of the aPDFA amounted to 92%, and for the recurvature deformities it was 90%.
The average value of the femoral extension was 47 ± 12 mm. The average distraction time was 38 ± 14 days. The period of deformity correction lasted 8 ± 6 days for simple deformities (SD), whereas it was 14 ± 7 days for moderate complexity deformities (MC), and 23 ± 12 days for complex deformities (CD).
The EFI for SD was 26 ± 8 days/cm, for MC it was 31 ± 6 days/cm, and for CD it was 35 ± 12 days/cm.
During the correction of femoral deformities, 48 (50.5%) complications occurred (Table 4). Most complications (71% of the total number of complications) were of Caton grade I. The remaining complications (29% of the total number of complications) were of Caton grade II. No complications of Caton grade III occurred.
Thus, in 18 of these cases (19%), soft tissue inflammation at the site of the outlet of the transosseous elements occurred. To reduce inflammation, antibiotic therapy was used in 8 cases and was effective in 6 of those cases; however, it was ineffective in 2 cases and required removal of the transosseous element. In the remaining 10 cases, the inflammation was arrested using dressings with various surface antiseptics and antibiotics. No cases of deep infection were observed in this group.
In 17 cases (18%) knee joint contracture occurred after the EFD removal. In 14 of those patients, the segment extension exceeded 5 cm. Surgical treatment of contractures was indicated for only 3 patients; satisfactory range of motion was achieved in the remaining patients through the active rehabilitation and remedial treatment.
Table 3. The reference lines and angles in the correction of tibia deformity
Indicator | Normal values | Before the treatment | After the treatment |
Frontal view | |||
Varus | |||
MAD, mm | 0–9,7 medially | 39 ± 10 medially | 4 ± 5 medially |
mMPrAT, ° | 85–90 | 78 ± 9 | 86 ± 8 |
mLDAT, ° | 86–92 | 97 ± 8 | 87 ± 4 |
Valgus | |||
MAD, mm | 0–9,7 medially | 21 ± 12 laterally | 1 ± 4 medially |
mMPrAT, ° | 85–90 | 98 ± 8 | 90 ± 5 |
mLDAT, ° | 86–92 | 78 ± 6 | 86 ± 4 |
Sagittal plane | |||
Antecurvature | |||
aPPTA, ° | 77–84 | 72 ± 7 | 79 ± 5 |
aADTA, ° | 78–82 | 85 ± 9 | 81 ± 6 |
Recurvation | |||
aPPTA, ° | 77–84 | 94 ± 8 | 84 ± 4 |
aADTA, ° | 78–82 | 71 ± 9 | 79 ± 6 |
Note: mMPrAT is the mechanical medial proximal angle of the tibia; mLDAT is the mechanical lateral distal angle of the tibia; MAD is the mechanical axis deviation; aPPTA is the anatomical posterior proximal tibial angle; aADTA is the anatomical anterior distal tibial angle.
Table 4. Complications of the treatment
Complication | Femur | Tibia |
Soft tissue inflammation in the site of outlet of the transosseous elements | 18 (19 %) | 14 (10 %) |
Joint contracture | 17 (18 %) | 12 (9 %) |
Fracture of the transosseous elements | 4 (4 %) | 5 (4 %) |
Pseudarthrosis or atrophic regenerate formation | 1 (1 %) | 3 (2 %) |
Secondary fractures and deformities | 0 (0 %) | 3 (2 %) |
Relapse of the deformity with the growth of the pediatric patient | 8 (8,5 %) | 25 (18 %) |
Total | 48 (50,5 %) | 62 (45 %) |
In 4 cases (4%), the spokes or rod-screws were broken internally; however, this did not have an impact on the functional result of treatment in any patients. In one case, the formation of atrophic regenerate occurred in a patient with the post-traumatic deformity of the femur. Additional intervention was required to restore bone integrity (e.g., bone grafting of the atrophic regenerate region with iliac crest auto-bone). In 4 cases (4%), the regenerate fracture occurred after EFD dismantling. In all cases, fracture treatment was performed conservatively with the plaster immobilization. In two of these patients, further surgical treatment of the deformities was required.
In 8 patients (8.5%), relapse of the deformity occurred during a patient’s growth spurt. It should be noted that these patients were all under the age of 12 years. Hematogenous osteomyelitis was diagnosed in 5 patients, congenital malformation of the femur was diagnosed in 2 patients, and Ollier’s disease was diagnosed in 1 patient. Repeated osteotomy and instrumental correction was indicated in 2 patients due to the relapse of the deformity. Osteotomy and intramedullary fixation was performed in 4 of these patients. Temporary hemiepiphysiodesis with figure-of-eight plates was used effectively in the remaining 2 patients.
Group 2. The results of the correction of tibial bone deformities are shown in Table 3. Thus, during the correction of varus deformities, the MAD average value was 4 ± 5 mm inwards, whereas in the valgus deformity correction it was 4 ± 1 mm inwards. The postoperative change in the MAD value compared with the preoperative value averaged 35 mm for varus deformities and 20 mm for valgus deformities. The accuracy of the deformity correction for the MAD was 93%.
The magnitude of the angular correction of the tibia in the frontal view was 25 ± 11º for varus deformities and 12 ± 6º for valgus deformities. The correction accuracy of the mMPrAT and mLDAT was 92% for varus deformities and 89% for valgus deformities.
The magnitude of the angular correction of the tibia in the sagittal plane was 16 ± 7º for the antecurvature deformities and 12 ± 9º for the recurvature deformities. The correction accuracy of the aPPTA and aADTA for the antecurvature deformities was 90%, whereas for the recurvature deformities it was 95%.
The average length of the tibial bone extension was 52 ± 20 mm. The distraction time was on average 45 ± 18 days. The period of the deformity correction was 11 ± 5 days for SD, 16 ± 9 days for MC, and 27 ± 16 days for CD. The EFI was 32 ± 14 days/cm for SD, 42 ± 12 for MC, and 49 ± 8 for CD.
There were 62 (45%) complications noted for tibial deformity corrections (Tables 4). Of those complications, 50% were of Caton grade I and 50% were of Caton grade II. No serious complications (Caton grade III) were registered.
Thus, in 14 cases (10%), soft tissue inflammation occurred at the site of outlet of the transosseous elements. Antibiotic therapy was indicated in 2 cases, and in all cases, the inflammation was arrested with dressings with various surface antiseptics and antibiotics. In 12 cases (9%), contracture of the ankle joint occurred after the EFD removal. Surgical treatment of contractures was indicated for 2 patients (achillotenotomy and fixation of the foot with the plaster cast); a satisfactory range of motion was achieved in the remaining patients through the active rehabilitation and remedial treatment.
In 5 cases (4%), the spoke or rod-screw was broken internally; however, this did not have an impact on the functional result of treatment in any patients. In 4 patients, the formation of atrophic regenerate occurred. Only one of these cases required additional intervention. In 3 cases (2%), the regenerate fracture occurred after the EFD dismantling. In both cases, the fracture treatment was performed conservatively with the plaster immobilization. Further surgical treatment was indicated for all of these patients.
In 25 patients (18%), relapse occurred during a growth spurt. Consolidated tibia pseudarthrosis was diagnosed in 14 patients, Blount disease in 6 patients, and congenital malformation of the tibia in 4 patients. It should be noted that the deformity relapses were predictable, given the nature of these abnormalities, the damage in the growth areas by the pathological process, or the asymmetry of the growth areas function. Follow-up was thorough, which enabled the prevention of the deformity’s progression through timely and minimally invasive interventions. Thus, in 20 out of 25 cases, hemiepiphysiodesis with the figure-of-eight plates and screws was performed, which had excellent results for all patients. It should be noted that hemiepiphysiodesis had been indicated for 8 patients prior to the EFD dismantling. In 3 cases, repeated osteotomy and instrumental correction was required. In 2 cases, osteotomy and intramedullary fixation using the rod with locking were performed.
Discussion
It is known that deformities of the lower limbs may result in the development of osteoarthritis [22, 23]. The accurate recovery of the limb anatomy and the RLA normalization reduces the risk of development and progression of this disease [24].
In the present study, 90 to 96% accuracy was achieved for the correction of femoral deformities, and 89 to 95% accuracy was achieved for the correction of tibial deformities. In general, these figures are consistent with the results of other prior studies.
Thus, P.V. Skomoroshko (2014) [11] provides data on the accuracy of the femoral deformity correction using the Ortho-SUV Frame in adults with average values of 90.4%. According to Manner et al. (2007) [10], Dammerer et al. (2011) [13], and Eidelman et al. (2006) [14], the accuracy of the correction of long bone deformities using another transosseous software-assisted unit, the Taylor apparatus, was 86 to 94%.
An interesting fact was that despite the small differences in the average values of extension length and period of deformity correction in both study groups, there was a significant difference in the EFI between femur and the tibia deformities. Thus, in the correction of the tibial deformities of moderate severity, the EFI exceeded that of the femur by an average 11 days/cm (p < 0.05). For the correction of complex deformities of the tibia, the EFI exceeded that of for the femur by an average 14 days/cm (p < 0.05). Park et al. (2015) [25] provided data that conflicts in some aspects with our results. For example, in their study the EFI was 42.5 days/cm for femoral deformities and 23 days/cm for tibia deformities. However, the conflicting results are most likely due to the fact that their study analyzed the results of the deformity correction only in patients with achondroplasia. In the study of Marangoz et al. (2008) [26], which utilized the Taylor apparatus, reported EFI values of 2.2 months/cm, which is almost 2 times higher than the EFI obtained in the present study.
In the analysis of the complications in the present study, it should be noted that the rate of complications was consistent with those typically expected for transosseous osteosynthesis: 50.5% for deformities of the femur and 45% for deformities of the tibia. However, serious complications that impaired functional outcome were not seen. In the femoral deformity correction group, only 29% of the total number of complications (14 patients) were of the Caton type II classification, that is, unforeseen additional surgery was necessary to remove the consequences of the complications. In the tibial deformity group, there were 31 such patients (50% of the total number of complications).
The most typical complication of the transosseous osteosynthesis is the inflammation of soft tissues at the site of outlet of the transosseous elements. The literature sources provide various data on the rate of this complication, which ranges from 8 to 96% [10, 11, 13, 26]. This discrepancy may be due to clinician subjectivity. It should be noted that in all patients soft tissue inflammation was arrested with either topical treatment or antibacterial therapy. The removal of the transosseous element was not required in any cases. Additionally, soft tissue inflammation was seen almost 2 times more frequently in the femoral deformity correction. The femoral extension also resulted in the formation of adjacent joints contractures 2 times more often than did the extension of the tibia.
Relapse of deformities is most characteristic of pediatric patients who are continuing to grow. This is due to partial damage to the growth zones or to their asymmetric functioning. In our study, this type of complication was observed more than 2 times more often in the correction of tibial deformities (8.5% for the femoral deformities, versus 18% for the tibial deformities). To avoid this type of complication, Koren et al. (2016) [27] recommend performing an epiphysiodesis of the intact part of the growth zone. However, this recommendation is feasible not in all cases of deformities in children; for example, it is impossible in children with asymmetrical functioning of the growth zone (e.g. fibular hemimelia or achondroplasia) or in small children. So, in our opinion, in some cases of partial damage in the growth zone (e.g. Blount disease, posttraumatic deformities with damage in the growth zone, the consequences of hematogenous osteomyelitis) or its asymmetrical functioning (fibular hemimelia, congenital malformation of the femur, achondroplasia), it is reasonable to perform a preventive temporary hemiepiphysiodesis when removing the transosseous apparatus.
Clinical example
Patient G., 10 years old, was admitted to the clinic of the Turner Scientific and Research institute for Children’s Orthopedics with the diagnosis of the Blount-Barber disease of the left lower extremity. At admission, the patient complained of a deformity of the left lower limb and limp. Previously, the patient twice received corrective osteotomies of the left tibia at other medical institutions . The last surgery was performed 1 year prior to this hospitalization. The child’s parents noticed that the deformity had increased 3 months after the last surgery. After the examination and analysis of panoramic radiographs (Fig. 1, a, b) it was revealed that the child had a complex varus-torsion deformity of the left tibia. Additionally, radiographs and CT revealed partial damage (“arrest”) of the growth zone that extended for approximately 50% of the medial portion of the proximal epiphysis. Before correction, the proximal medial tibial mechanical angle was 36º, the distal lateral tibial mechanical angle was 93º, the anatomical dorsal proximal tibial angle was 71º, and the mechanical axis deviation was 272 mm inwards. The varus deformity angle was 54º, the angle of the antecurvature deformity was 10º, and the angle of internal tibial torsion was 40º. The deformity correction was planned on the reference lines and skiagrams, as well as the “simulation” of the correction and osteosynthesis (Fig. 1, c, d).
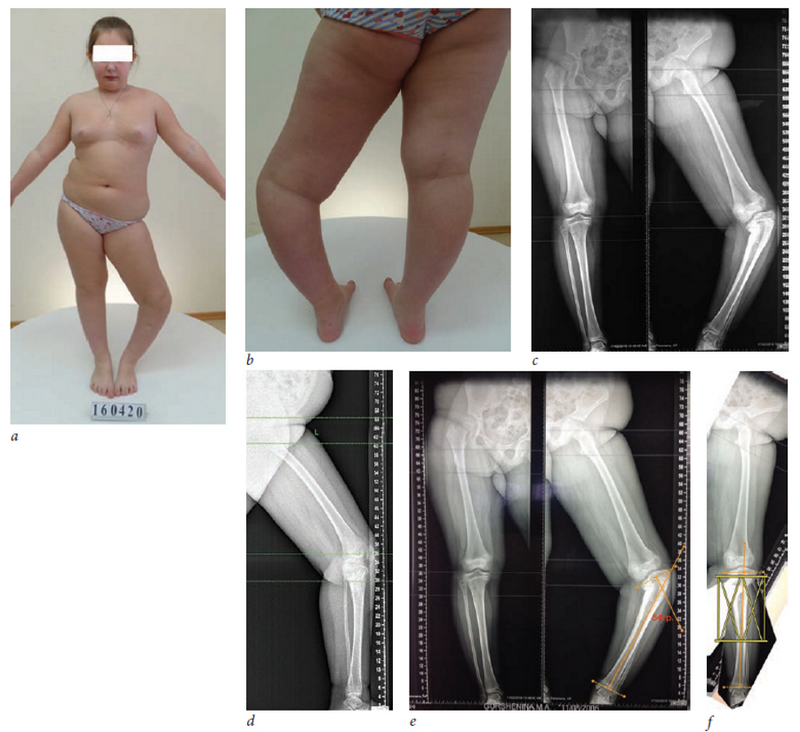
Fig. 1. The patient G. before the treatment: a, b - the appearance; c, d - teleroentgenograms of the lower extremities; e - the mechanical axes of the proximal and distal bone fragments were performed on the radiograph, the apex and the angle of deformity were found; f - the “simulating” osteotomy of the skiagram at the apex level was performed using the BoneNinja program, the deformity is eliminated, and the installation of the hexapod is simulated.
Considering the deformity location, history of deformity relapses shortly after the previous surgeries, damage to the medial portion of the proximal growth zone of the tibia with the preserved function of the lateral portion, the surgical plan of care included the following: epiphysiodesis of the outer portion of the proximal growth zone using the drill, a corticotomy with osteoclasis of the upper third of the left tibia bone, and the combined transosseous osteosynthesis using the Ortho-SUV Frame (Fig. 2, a, b). Given the height of the osteotomy, the knee joint was fixed.
In the postoperative period, the deformity correction was calculated in the computer navigation program for the Ortho-SUV Frame (Fig. 2, c). And using the program tools the axes of the proximal and distal fragments in frontal and lateral projections were built, skiagrams were made. Also, an “over-elongation” of the segment by 1 cm was programmed. The selected rate of the correction was 1 mm/day. The correction was performed fractionally 4 times/day while observing the “gold standard” of distraction by the Ilizarov frame and using the original telescopic racks (strata) of the Ortho-SUV Frame.

Fig. 2. The patient G. after the surgery: a - appearance of the limb after the surgery; b - the X-ray data after the surgery; c - the calculation of the deformity correction in the program of the Ortho-SUV Frame, at the step 11, where the yellow contour is a skiagram of the distal bone fragment at the time of the calculation, the red contour is the expected final position of the distal bone fragment after the deformity correction.
The deformity was eliminated in one stage over a period of 48 days (Fig. 3, a, b). Upon completion of the correction, the support was dismantled from the lower third of the femur and the knee joint was “unlocked”. Active range of motion was initiated in the left knee at that time. The EFD was dismantled 171 days after surgery (Fig. 4). The external fixation index was 31 days/cm and the following parameters of the reference lines and angles were achieved: mMPrAT was 87º, mLDAT was 90º, aPPTA was 80º, aADTA was 82º, and MAD was 0 mm.

Fig. 3. Photos and panoramic radiographs of the patient G.: a - the radiographs after the correction of the deformity; b - after dismantling the support from the lower third of the femur
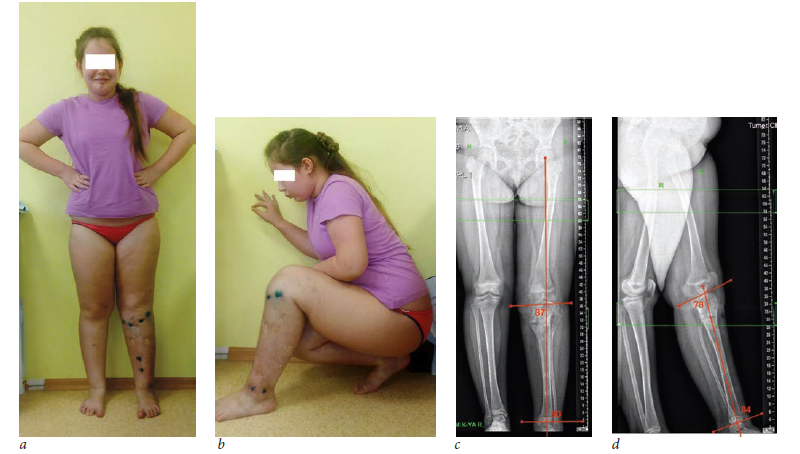
Fig. 4. Photos and panoramic radiographs of patient G. after the dismantling of the external fixation device
Conclusion
The results of the present study indicate that the use of the software-assisted Ortho-SUV Frame is extremely accurate for the transosseous osteosynthesis correction of long bones deformities that are accompanied by shortening in pediatric patients. The use of this technique is equally effective for the correction of femoral and tibial deformities. It should be considered that accurate correction of deformities in pediatric patients is not an guarantee of successful treatment due to the ongoing “impaired” functioning of the growth zones damaged by the pathological process or injury. In this regard, the use of the instrumental correction must often be combined with the intervention in the growth zone (controlled growth, epiphysiodesis etc.).
Information on funding and conflict of interest
Vilensky V.A. declares that he is an employee of the company LLC “Ortho-SUV”.
作者简介
Viktor Vilensky
The Turner Scientific and Research Institute for Children’s Orthopedics
编辑信件的主要联系方式.
Email: vavilensky@mail.ru
MD, PhD, senior research associate of the department of bone pathology 俄罗斯联邦
Andrey Pozdeev
The Turner Scientific and Research Institute for Children’s Orthopedics
Email: aapozdeev@gmail.com
MD, PhD, orthopedic and trauma surgeon of the department of bone pathology 俄罗斯联邦
Timur Zubairov
The Turner Scientific and Research Institute for Children’s Orthopedics
Email: fake@eco-vector.ru
MD, PhD, research associate of the department of bone pathology 俄罗斯联邦
Ekaterina Zakharyan
The Turner Scientific and Research Institute for Children’s Orthopedics
Email: zax-2008@mail.ru
MD, orthopedic and trauma surgeon 俄罗斯联邦
Aleksander Pozdeev
MD, PhD, professor, chief research associate of the department of bone pathology
Email: prof.pozdeev@mail.ru
The Turner Scientific and Research Institute for Children’s Orthopedics 俄罗斯联邦
参考
- Илизаров Г.А., Зырянов С.Я. Коррекция деформаций сегментов нижней конечности с одновременным удлинением ее по Илизарову. Метод Илизарова: теория, эксперимент, клиника: тез. докл. юбилейной международ. конф. — Курган, 1991. — С. 287–289. [Ilizarov GA, Zyrjanov SJa. Korrekcija deformacij segmentov nizhnej konechnosti s odnovremennym udlineniem ee po Ilizarovu. Metod Ilizarova: teorija, jeksperiment, klinika. [conference proceedings] Kurgan; 1991. P. 287-289. (In Russ.)]
- Ilizarov GA. Transosseous osteosynthesis. Theoretical and clinical aspects of the regeneration and growth of tissue. Springer-Verlag Berlin, Heidelberg, New York, 1992. 800 p. doi: 10.3109/17453679209154834.
- Соломин Л.Н. Основы чрескостного остеосинтеза. Частные вопросы – 2. — Т. 2. — 2-е изд., перераб. и доп. — М.: БИНОМ, 2015. — 560 с. [Solomin LN. Osnovy chreskostnogo osteosinteza. Chastnye voprosy – 2. Vol. 2. Moscow: BINOM; 2015. 560 p. (In Russ.)]
- Голяховский В., Френкель В. Руководство по чрескостному остеосинтезу методом Илизарова: Пер. с англ. — М.: БИНОМ, 1999. — 272 с. [Goljahovskij V, Frenkel’ V. Rukovodstvo po chreskostnomu osteosintezu metodom Ilizarova. Translation from English. Moscow: BINOM; 1999. 272 p. (In Russ.)].
- Ли А.Д., Попков А.В., Грачева В.И., и др. Возможности чрескостного остеосинтеза по Илизарову в ликвидации укорочения у взрослых и детей. Экспериментально-теоретические и клинические аспекты разрабатываемого в КНИИЭКОТ метода чрескостного остеосинтеза: материалы Всесоюз. симпоз. с участ. иностр. специал. — Курган, 1984. — C. 177–181. [Li AD, Popkov AV, Gracheva VI, et al. Vozmozhnosti chreskostnogo osteosinteza po Ilizarovu v likvidacii ukorochenija u vzroslyh i detej. Jeksperimental’no-teoreticheskie i klinicheskie aspekty razrabatyvaemogo v KNIIJeKOT metoda chreskostnogo osteosinteza. [conference proceedings] Kurgan, 1984. P. 177-181. (In Russ.)]
- Hsu RWW, et al. Normal axial alignment of lower extremity and load-bearing distribution at the knee. Clin Orthop Clinical and Rel Res. 1990;255:215-227. doi: 10.1097/00003086-199006000-00029.
- Paley D. Principles of deformity correction. New York: Springer-Verlag; 2005. 806 p.
- Соломин Л.Н., Щепкина Е.А., Кулеш П.Н., и др. Определение референтных линий и углов длинных трубчатых костей: пособие для врачей / РНИИТО им. Р.Р. Вредена. — СПб., 2010. — 48 с. [Solomin LN, Shhepkina EA, Kulesh PN, et al. Opredelenie referentnyh linij i uglov dlinnyh trubchatyh kostej: posobie dlja vrachej / RNIITO named after R.R. Vredena. Saint Petersburg; 2010. 48 p. (In Russ.)]
- Eren I, Eralp L, Kocaoglu M. Comparative clinical study on deformity correction accuracy of different external fixators . Int Orthop (SICOT). 2013;37(11):2247. doi: 10.1007/s00264-013-2116-x.
- Manner HM, Huebl M, Radler C, et al. Accuracy of complex lower-limb deformity correction with external fixation: a comparison of the Taylor spatial frame with the Ilizarov ring fixator. J Child Orthop. 2007;1(1):55. doi: 10.1007/s11832-006-0005-1.
- Скоморошко П.В. Оптимизация лечения больных с диафизарными деформациями бедренной кости на основе использования чрескостного аппарата со свойствами пассивной компьютерной навигации: дис. … канд. мед. наук. — СПб., 2014. — 224 с. [Skomoroshko PV. Optimizacija lechenija bol’nyh s diafizarnymi deformacijami bedrennoj kosti na osnove ispol’zovanija chreskostnogo apparata so svojstvami passivnoj komp’juternoj navigacii [dissertation]. Saint Petersburg; 2014. (In Russ.)]
- Соломин Л.Н., Щепкина Е.А., Виленский В.А., и др. Коррекция деформаций бедренной кости по Илизарову и основанным на компьютерной навигации аппаратом «Орто-СУВ» // Травматология и ортопедия России. — 2011. — № 3. — С. 32–39. [Solomin LN, Shhepkina EA, Vilenskij VA, et al. Correction of femur deformities by Ilizarov method and by apparatus Ortho-SUV based on computer navigation. Traumatology and Orthopedics of Russia. 2011;(3):32-39. (In Russ.)]. doi: 10.21823/2311-2905-2011-0-3-32-39.
- Dammerer D, Kirschbichler K, Donnan L, et al. Clinical value of the Taylor Spatial Frame: a comparison with the Ilizarov and Orthofix fixators. J Child Orthop. 2011;5(5):343. doi: 10.1007/s11832-011-0361-3.
- Eidelman M, Bialik V, Katzman A. Correction of deformities in children using the Taylor spatial frame. J Pediatr Orthop B. 2006;15(6):387-395. doi: 10.1097/01.bpb.0000228380.27239.8a.
- Paley D. History and Science Behind the Six-Axis Correction External Fixation Devices in Orthopaedic Surgery. Oper Tech Orthop. 2011;21:125-128. doi: 10.1053/j.oto.2011.01.011.
- Виленский В.А., Поздеев А.П., Бухарев Э.В., и др. Ортопедические гексаподы: история, настоящее, перспективы // Ортопедия, травматология и восстановительная хирургия детского возраста. — 2015. — T. 3. — № 1. — C. 61–69. [Vilenskij VA, Pozdeev AP, Buharev EV, et al. Orthopedic hexapods: history, present and prospects. Pediatric traumatology, orthopaedics and reconstructive surgery. 2015;3(1):61-69. (In Russ.)]. doi: 10.17816/PTORS3161-69.
- Соломин Л.Н., Виленский В.А., Утехин А.И., Террел В. Сравнительный анализ репозиционных возможностей чрескостных аппаратов, работающих на основе компьютерной навигации и аппарата Илизарова // Гений ортопедии. — 2009. — № 1. — С. 5–10. [Solomin LN, Vilensky VA, Utekhin AI, Terrel V. The comparative analysis of the reposition potentials of transosseous devices operating on the basis of computer navigation and the Ilizarov fixator. Genij Ortopedii. 2009;(1):5-10. (In Russ.)].
- Соломин Л.Н., Виленский В.А., Утехин А.И., Террел В. Сравнительный анализ жесткости остеосинтеза, обеспечиваемой чрескостными аппаратами, работающими на основе компьютерной навигации, и комбинированным спицестержневым аппаратом // Травматология и ортопедия России. — 2009. — № 2 — С. 20–25. [Solomin LN, Vilenskij VA, Utehin AI, Terrel V. Sravnitel’nyj analiz zhestkosti osteosinteza, obespechivaemoj chreskostnymi apparatami, rabotajushhimi na osnove komp’juternoj navigacii i kombinirovannym spice-sterzhnevym apparatom. Travmatologija i ortopedija Rossii. 2009;(2):20-25. (In Russ.)]
- Solomin LN, Paley D, Shchepkina EA, et al. A comparative study of the correction of femoral deformity between the Ilizarov apparatus and Ortho-SUV Frame. Int Orthop (SICOT). 2014;38:865. doi: 10.1007/s00264-013-2247-0.
- Соломин Л.Н., Виленский В.А. Практическая классификация деформаций длинных трубчатых костей // Травматология и ортопедия России. — 2008. — № 3 (Приложение). — С. 44. [Solomin LN, Vilenskij VA. Prakticheskaja klassifikacija deformacij dlinnyh trubchatyh kostej. Travmatologija i ortopedija Rossii. 2008;(3)(prilozhenie):44 (In Russ.)]
- Caton J. L’allongement bilatéral des membres inférieurs chez les sujets de petite taille en France. Résultats de l’enquête GEOP; notre expérience: Traitement des inegalites de longueur des membres inferieurs et des sujets de petite taille chez l’enfant et l’adolescent: Sym-posium sous la direction de J. Caton (Lyon). Rev Chir Orthop. 1991;77(1):74-77.
- Kettelkamp DB, Hillberry BM, Murrish DE, Heck DA. Degenerative arthritis of the knee secondary to fracture malunion. Clin Orthop Relat Res. 1988;234:159-169. doi: 10.1097/00003086-198809000-00029.
- Probe RA. Lower extremity angular malunion. J Am Acad Orth Surg. 2003;11:302-311.
- Sharma L, Eckstein F, Song J, et al. Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum. 2008;58(6):1716-1726. doi: 10.1002/art.23462.
- Park K-W, Garcia RN, Rejuso CA, et al. Limb Lengthening in Patients with Achondroplasia. Yonsei Medical Journal. 2015;56(6):1656-1662. doi: 10.3349/ymj.2015.56.6.1656.
- Marangoz S, Feldman DS, Sala DA, et al. Femoral deformity correction in children and young adults using Taylor spatial frame. Clin Orthop Relat Res. 2008;466(12):3018. doi: 10.1007/s11999-008-0490-2.
- Koren L, Keren Y, Eidelman M, Koren L. Multiplanar deformities correction using Taylor Spatial Frame in skeletally immature patients. Open Orthop J. 2016;10:71-79. doi: 10.2174/1874325001610010603.
补充文件