Нейросегментарный уровень и его значение при лечении подвывиха и вывиха бедра у детей с последствиями спинномозговых грыж
- Авторы: Баиндурашвили А.Г.1, Иванов С.В.1, Кенис В.М.1
-
Учреждения:
- ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
- Выпуск: Том 4, № 4 (2016)
- Страницы: 6-11
- Раздел: Статьи
- Статья получена: 28.12.2016
- Статья одобрена: 10.01.2017
- Статья опубликована: 14.12.2016
- URL: https://journals.eco-vector.com/turner/article/view/5889
- DOI: https://doi.org/10.17816/PTORS446-11
- ID: 5889
Цитировать
Аннотация
Актуальность. Патология тазобедренного сустава у детей с последствиями спинномозговых грыж является частым сопутствующим состоянием и в подавляющем большинстве случаев сопровождается формированием подвывиха и вывиха бедра.
Цель исследования — определение влияния нейросегментарного уровня на результаты хирургического лечения подвывиха и вывиха бедра у детей с последствиями спинномозговых грыж.
Материалы и методы. В ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России в период с 2006 по 2015 год проведено обследование и лечение 114 пациентов с подвывихом и вывихом бедра с последствиями спинномозговых грыж. Основная группа представлена 62 пациентами, которые получили хирургическое лечение, направленное на стабилизацию тазобедренного сустава. Контрольная группа — 52 ребенка, которые хирургического лечения по поводу подвывиха и вывиха бедра не получили. Внутри каждой группы пациенты распределены на две подгруппы в зависимости от нейросегментарного уровня поражения спинного мозга, используя методику Sharrаrd.
Результаты. У пациентов основной группы с высокими нейросегментарными уровнями (грудной и L1-L2) хирургическое лечение подвывиха и вывиха бедра в большинстве случаев (16 из 22, то есть 72 %) привело к ухудшению двигательного уровня (архивный материал); у пациентов с нейросегментарными уровнями L3-L4 и L5-S1 в 13 из 40 случаев (32,5 %) двигательный уровень улучшился, в то время как у пациентов контрольной группы двигательные возможности ухудшились в 10 из 28 (36 %) случаев.
Заключение. Определение нейросегментарного уровня позволяет прогнозировать двигательный
Ключевые слова
Полный текст
Введение
Спинномозговые грыжи возникают вследствие комбинированного порока эмбрионального развития нервной системы и сопровождаются сложным комплексом клинических проявлений как со стороны позвоночника и спинного мозга, так и со стороны опорно-двигательного аппарата, мочеполовой и других систем.
Ортопедические проявления спинномозговых грыж могут носить врожденный характер, а также формироваться и прогрессировать в процессе постнатального роста и развития ребенка. Врожденные ортопедические проявления спинномозговых грыж включают порок развития позвоночника, контрактуры суставов и деформации нижних конечностей, выявляемые непосредственно после рождения. Их причиной является внутриутробное влияние неврологического дефицита на пренатальное развитие. В то же время большинство ортопедических нарушений имеют закономерную динамику в постнатальном периоде. Процесс формирования ортопедических последствий спинномозговой грыжи характеризуется чертами, свойственными патогенезу всех деформаций паралитического происхождения. Основными его определяющими факторами являются мышечный дисбаланс, трофические нарушения, отягощающее влияние статико-динамических факторов, отсутствие ортопедической профилактики развития деформаций [1–3].
Патология тазобедренного сустава у детей с последствиями спинномозговых грыж является частым сопутствующим состоянием и в подавляющем большинстве случаев сопровождается формированием подвывиха и вывиха бедра. По данным различных авторов, у 30–50 % детей с последствиями спинномозговых грыж подвывих или вывих в тазобедренном суставе развиваются в течение первых 2–3 лет жизни [4]. Большинство исследователей связывает формирование подвывиха и вывиха в тазобедренном суставе с характером первичного поражения сегментарного аппарата спинного мозга, а именно с нейросегментарным уровнем [5].
Под нейросегментом (в отечественной литературе чаще используется термин «сегмент») понимается определенный участок спинного мозга в горизонтальной плоскости, дающий начало одной паре спинномозговых нервов [6]. Как в зарубежной, так и в отечественной литературе все чаще встречаются публикации о влиянии нейросегментарного уровня последствий спинномозговой грыжи на тактику лечения ортопедических нарушений [7–9].
Цель настоящего исследования — определение влияния нейросегментарного уровня на результаты хирургического лечения подвывиха и вывиха бедра у детей с последствиями спинномозговых грыж.
Материалы и методы
В ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России в период с 2006 по 2015 год проведено обследование и лечение 114 пациентов с последствиями спинномозговых грыж с подвывихом и вывихом бедра. Все пациенты и/или их родители (опекуны) добровольно подписали информированное согласие на участие в исследовании и выполнение хирургического вмешательства. Для оценки соотношений в тазобедренном суставе мы использовали стандартные и функциональные рентгенологические проекции. В качестве показателя, определяющего градации степени рентгенологических нарушений в тазобедренном суставе, мы пользовались наиболее распространенным критерием для фронтальной плоскости — индексом миграции. Для определения подвывиха бедра мы считали значение индекса миграции более 40 %. Вывих бедра характеризовался полным разобщением ацетабулярной и бедренной суставных поверхностей.
Исследование построено на сравнительном анализе результатов обследования и лечения пациентов двух групп — основной и контрольной. Основная группа представлена 62 пациентами, которые получили хирургическое лечение, направленное на стабилизацию тазобедренного сустава, контрольная группа — 52 детьми, которым хирургическое лечение по поводу подвывиха и вывиха бедра не осуществлялось.
С целью устранения подвывиха и вывиха бедра нами выполнялись реконструктивные операции, включавшие в себя вмешательства на бедренном и тазовом компонентах сустава. Остеотомия бедренной кости выполнялась во всех случаях реконструкции сустава по общепринятой методике с учетом исходных параметров шеечно-диафизарного угла и угла антеторсии. Коррекция изменений тазового компонента сустава производилась с учетом возраста пациента, показателей ацетабулярного индекса, а также изменения значения угла заднего края вертлужной впадины.
При обследовании определялся нейросегментарный уровень по классификации Sharrаrd [10]. Она основана на принципе оценки силы (в баллах) основных мышечных групп нижних конечностей, иннервирующихся соответствующим нейросегментом (табл. 1).
Таблица 1. Классификация двигательных нарушений по нейросегментарному уровню Sharrаrd
Уровень | Мышечная сила | Нейросегментарный уровень |
1-й | Сила подошвенных сгибателей стопы (4–5 баллов) | S2 |
2-й | Сила подошвенных сгибателей стопы (менее 3 баллов) Сила сгибателей голени (3 балла) Сила разгибателей и /или отводящих мышц бедра (2–3 балла) | S1-L5 |
3-й | Сила сгибателей бедра (4–5 баллов) Сила сгибателей голени (менее 3 баллов) Сила разгибателей и отводящих мышц бедра (1–2 балла) | L4-L3 |
4-й | Отсутствие активного разгибания в коленном суставе Сила сгибателей бедра (приводящих мышц) (менее 2 баллов) Поднятие таза (3–4 балла) | L2-L1 |
5-й | Отсутствие мышечной активности нижних конечностей. Отсутствие способности приподнять таз над опорной поверхностью в горизонтальном положении | Грудной |
С учетом нейросегментарного уровня нами выделены две клинические подгруппы в основной и контрольной группах пациентов:
- пациенты с высокими нейросегментарными уровнями — грудной и L1-L2;
- пациенты с низкими нейросегментарными уровнями — L3-L4, L5-S1.
До 2009 года критерием включения в основную группу детей, подвергшихся оперативному лечению, являлось наличие подвывиха или вывиха бедра независимо от нейросегментарного уровня (подгруппу 1 составил архивный материал), а критерием включения в контрольную группу пациентов, не подвергавшихся оперативному лечению, являлось наличие декомпенсированной соматической патологии или отказ родителей от хирургического лечения. После 2009 года критерием включения в основную группу было наличие подвывиха и вывиха бедра при нейросегментарных уровнях L3-L4 и L5-S1, а критерием включения в контрольную группу — противопоказания к оперативному лечению в связи с наличием подвывиха или вывиха бедра у пациентов с грудным и L1-L2 нейросегментарными уровнями, соматической патологии или в связи с отказом родителей от хирургического лечения.
На рис. 1 представлено распределение пациентов в основной и контрольной группах.
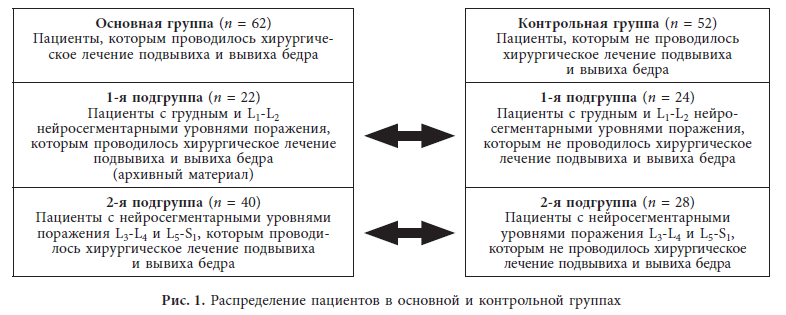
Основная группа (n = 62) Пациенты, которым проводилось хирургическое лечение подвывиха и вывиха бедра | Контрольная группа (n = 52) Пациенты, которым не проводилось хирургическое лечение подвывиха и вывиха бедра | |
1-я подгруппа (n = 22) Пациенты с грудным и L1-L2 нейросегментарными уровнями поражения, которым проводилось хирургическое лечение подвывиха и вывиха бедра (архивный материал) | 1-я подгруппа (n = 24) Пациенты с грудным и L1-L2 нейросегментарными уровнями поражения, которым не проводилось хирургическое лечение подвывиха и вывиха бедра | |
2-я подгруппа (n = 40) Пациенты с нейросегментарными уровнями поражения L3-L4 и L5-S1, которым проводилось хирургическое лечение подвывиха и вывиха бедра | 2-я подгруппа (n = 28) Пациенты с нейросегментарными уровнями поражения L3-L4 и L5-S1, которым не проводилось хирургическое лечение подвывиха и вывиха бедра |
У всех пациентов определялся двигательный уровень по методике, предложенной Мельбурнским медицинским университетом для детей с последствиями спинномозговых грыж, которая предполагает пять уровней двигательной активности (табл. 2).
Таблица 2. Оценка двигательных уровней пациентов с последствиями спинномозговой грыжи, предложенная Мельбурнским медицинским университетом
Функциональные возможности пациентов | Двигательный уровень |
Способность ходить не хуже сверстников | 5-й |
Ходьба с использование ортезов голеностопного сустава без дополнительных средств опоры. Использование коляски только на длинные дистанции | 4-й |
Ходьба в пределах дома при помощи ортезов и дополнительных средств опоры. Использование коляски как вне, так и внутри дома | 3-й |
Ходьба во время лечения, в школе и ограниченное время дома, использование коляски при передвижении | 2-й |
Отсутствие ходьбы | 1-й |
Оценка двигательного уровня проводилась у пациентов до и после лечения.
Результаты и обсуждение
На основании результатов обследования и лечения нами проведена сравнительная оценка динамики двигательного уровня у пациентов с грудным и L1-L2 нейросегментарными уровнями (1-я подгруппа) в основной и контрольной группах. Результаты представлены на рис. 2.

Как видно из данных, представленных на рис. 2, ни у одного ребенка основной группы двигательный уровень в результате лечения не улучшился, а у 16 из 22 (73 %) пациентов он ухудшился. Анализ возможных причин ухудшения двигательного уровня в послеоперационном периоде показал, что у 16 из 22 пациентов наблюдались спонтанные переломы длинных трубчатых костей нижних конечностей, обусловленные выраженным остеопорозом, что часто случается у пациентов с данной патологией.
Нами проведен сравнительный анализ частоты переломов у пациентов с грудным и L1-L2 нейросегментарными уровнями в основной и контрольной группах за период наблюдения. У детей основной группы количество переломов было значительно больше, чем в контрольной группе, у 14 из 16 (87 %) их было более двух. Для пациентов с последствиями спинномозговых грыж характерно появление переломов без наличия очевидного травматического фактора.
В контрольной группе двигательные возможности улучшились у 6 из 24 (25 %) пациентов. У 4 из 24 детей двигательные возможности ухудшились, и эти ухудшения также были связаны с переломами, полученными, как правило, в процессе проводимого восстановительного лечения. У остальных 14 пациентов двигательные возможности не изменились, и все они передвигались только в инвалидном кресле, у них отсутствовали контрактуры в тазобедренных суставах, которые мешали бы ребенку сидеть или лежать.
Таким образом, у пациентов с высокими нейросегментарными уровнями (грудной и L1-L2) хирургическое лечение подвывиха и вывиха бедра не только не привело к улучшению двигательного уровня, но и у большинства детей (в нашем исследовании — у 16 из 22, то есть у 72 %) основной группы состояние ухудшилось. Уменьшение двигательной нагрузки в послеоперационном периоде приводило к уменьшению костной плотности ткани, развитию остеопороза и формированию «каскада» переломов длинных трубчатых костей, что неминуемо вызывало ухудшение двигательных возможностей ребенка.
Также нами проведена сравнительная оценка динамики двигательного уровня у пациентов с нейросегментарными уровнями L3-L4 и L5-S1 в основной и контрольной группах (2-я подгруппа). Результаты представлены на рис. 3.

Как видно из данных, представленных на рис. 3, в результате хирургического лечения подвывиха и вывиха бедра в основной группе у 13 из 40 (32,5 %) пациентов двигательный уровень улучшился. У 23 из 40 (57,5 %) детей двигательный уровень сохранился на дооперационном уровне, причем у всех у них на момент операции имелся потенциально максимально возможный двигательный уровень, и своевременно выполненное хирургическое лечение позволило сохранить достигнутые двигательные возможности ребенка. В то же время у пациентов контрольной группы двигательные возможности ухудшились в 10 из 28 (36 %) случаев.
Таким образом, хирургическое лечение пациентов с подвывихом и вывихом бедра привело к улучшению двигательного уровня в 32,5 % случаев, в то же время отсутствие хирургического лечения в контрольной группе привело к ухудшению двигательного уровня у 36 % пациентов.
Полученные нами результаты лечения детей с последствиями спинномозговых грыж свидетельствуют о том, что именно нейросегментарный уровень определяет как показания к хирургическому лечению подвывиха или вывиха бедра, так и вероятный двигательный уровень ребенка.
Выводы
- При планировании хирургического лечения детей с последствиями спинномозговых грыж при наличии подвывиха и вывиха бедра нейросегментарный уровень и двигательный уровень определяют выбор тактики лечения.
- Хирургическое лечение подвывиха и вывиха бедра у детей при грудном и L1-L2 нейросегментарных уровнях не показано, так как не приводит к улучшению двигательного уровня.
- Хирургическое лечение подвывихов и вывихов в тазобедренном суставе у детей с нейросегментарными уровнями L3-L4 и L5-S1 приводит к улучшению двигательного уровня в 32,5 % случаев.
Информация о финансировании и конфликте интересов
Работа проведена при поддержке ФГБУ «НИДОИ им. Г. И. Турнера» Минздрава России. Авторы декларируют отсутствие явных и потенциальных конфликтов интересов, связанных с публикацией настоящей статьи.
Об авторах
Алексей Георгиевич Баиндурашвили
ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
Автор, ответственный за переписку.
Email: turner01@mail.ru
д-р мед. наук, профессор, академик РАН, заслуженный врач РФ, директор ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России Россия
Станислав Вячеславович Иванов
ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
Email: turner01@mail.ru
канд. мед. наук, научный сотрудник отделения патологии стопы, нейроортопедии и системных заболеваний Россия
Владимир Маркович Кенис
ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
Email: kenis@mail.ru
д-р мед. наук, заместитель директора по развитию и внешним связям, руководитель отделения патологии стопы, нейроортопедии и системных заболеваний Россия
Список литературы
- Asher M, Olson J. Factors affecting the ambulatory status of patients with spina bifida cysticа. J Bone Joint Surg Am. 1983;65(3):350-6.
- Correll J, Gabler C. The effect of soft tissue release of the hips on walking in myelomeningocele. J Pediatr Orthop B. 2000;9(3):148-153. doi: 10.1097/01202412-200006000-00003.
- Feiwell E, Sakai D, Blatt A. The effect of hip reduction on function in patients with myelomeningocele. Potential gains and hazards of surgical treatment. J Bone Joint Surg Am. 1978;60(2):169-73.
- Erol B, Bezer M, Kucukdarmaz F, et al. Surgical management of hip instabilities in children with spina bifida. Acta Orthop Traumatol Turc. 2005;39(1):16-22.
- Баиндурашвили А.Г., Иванов С.В., Кенис В.М. Подвывих и вывих бедра у детей с последствиями спинномозговых грыж (обзор литературы) // Травматология и ортопедия России. – 2013. – № 4. – С. 97–102. [Baindurashvili AG, Ivanov SV, Kenis VM. Subluxation and dislocation of the hip in children with spina bifida (Review). Traumatology and Orthopedics of Russia. 2013;(4):97-192. (In Russ.)]
- Бадалян Л.О. Невропатология. – М.: Просвещение, 1987. – 316 с. [Badalyan LO. Nevropatologiya. Moscow: Prosvechenie; 1987. 316 p. (In Russ.)]
- Иванов С.В., Кенис В.М., Икоева Г.А., и др. Использование роботизированной двигательной реабилитации в комплексном лечении подвывиха и вывиха бедра у детей с последствиями спинномозговой грыжи // Ортопедия, травматология и восстановительная хирургия детского возраста. – 2014. – Т. II. – Вып. 4. – С. 32–35. [Ivanov SV, Kenis VM, Ikoeva GA, et al. The use of robotic rehabilitation in complex treatment of subluxation and dislocation of the hip in children with sequelae of spina bifida. Pediatric Traumatology, Orthopaedics and Reconstructive Surgery. 2014;2(4):32-5. (In Russ.)]
- Thomson JD, Segal LS. Orthopedic managment of spina bifida. Dev Disabill Res Rev. 2010;16(1):96-103. doi: 10.1002/ddrr.97.
- Yildirim T, Gursu S, Bayhan İA, et al. Surgical treatment of hip instability in patients with lower lumbar level myelomeningocele: Is muscle transfer required? Clin Orthop Relat Res. 2015;473(10):3254-60. doi: 10.1007/s11999-015-4316-8.
- Sharrard WJW. The segmental innervation of the lower limb muscles in man. Ann R Coll Surg Engl. 1964;35:106-22.
Дополнительные файлы