Использование метода управляемого роста для устранения сгибательной контрактуры коленного сустава у пациентов с артрогрипозом: предварительные результаты
- Авторы: Трофимова С.И.1, Буклаев Д.С.1, Петрова Е.В.1, Мулеванова С.А.1
-
Учреждения:
- ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
- Выпуск: Том 4, № 4 (2016)
- Страницы: 64-70
- Раздел: Статьи
- Статья получена: 10.01.2017
- Статья одобрена: 10.01.2017
- Статья опубликована: 14.12.2016
- URL: https://journals.eco-vector.com/turner/article/view/5897
- DOI: https://doi.org/10.17816/PTORS4464-70
- ID: 5897
Цитировать
Аннотация
Введение. Сгибательные контрактуры коленных суставов у детей с артрогрипозом встречаются часто и значительно изменяют кинематику ходьбы, снижают эффективность передвижения или делают его невозможным. Из многообразия методов хирургического лечения — мягкотканный релиз с использованием аппарата Илизарова или без него, разгибательная надмыщелковая остеотомия бедренной кости — сложно выбрать наиболее эффективный, так как каждый метод имеет свои недостатки.
Целью исследования было оценить результаты коррекции сгибательных контрактур коленных суставов с помощью метода управляемого роста у пациентов с артрогрипозом.
Материалы и методы. В исследование было включено 12 пациентов с артрогрипозом со сгибательными контрактурами коленных суставов (20 коленных суставов), которым выполнялся временный гемиэпифизеодез передней части дистальной зоны роста бедренной кости с использованием 8-образных пластин. Средний возраст на момент операции составлял 6,5 ± 0,5 года (4,3–9,6). Применялся клинический и рентгенологический методы исследования со статистической обработкой полученных данных.
Результаты. Средняя величина дефицита разгибания коленного сустава до операции составляла 48,5 ± 4,04° (20–80°). За период наблюдения от 18 до 36 месяцев после гемиэпифизеодеза дистальной зоны роста бедренной кости было отмечено уменьшение сгибательной контрактуры коленного сустава в 17 случаях (85 %) в среднем на 20 ± 2,67° (0–40°), p < 0,05. Величина резидуальной деформации составила 28,5 ± 6,03° (0–60°). Наиболее значительно (на 90 % по сравнению с исходной величиной) происходила коррекция у пациентов с контрактурами до 50° (p < 0,05). В этой группе были пациенты с тяжелыми сгибательными контрактурами, которым до операции производилась попытка их коррекции гипсовыми повязками с дистракционным устройством, в результате чего величина контрактуры была значительно уменьшена.
Выводы. Метод временного гемиэпифизеодеза является эффективным, безопасным и менее инвазивным по сравнению с другими методиками и может применяться для лечения детей с артрогрипозом. Сочетание гемиэпифизеодеза с дополнительными методами коррекции сгибательной контрактуры помогает значительно уменьшить ее величину, перевести ее из тяжелой в умеренную, делая тем самым лечение более эффективным и менее продолжительным, что позволяет в кратчайшие сроки достичь вертикализации пациента.
Полный текст
Введение
Сгибательные контрактуры коленных суставов при артрогрипозе встречаются у 22–67 % детей [1–3]. Именно эти деформации значительно изменяют кинематику ходьбы, снижают комфорт передвижения или делают его невозможным [4, 5]. Лечение сгибательных контрактур коленных суставов у пациентов с артрогрипозом должно быть начато как можно раньше с применением специальных упражнений, этапных гипсовых повязок и последующего ортезирования [6]. Для лечения ригидных контрактур существуют различные хирургические методы: мягкотканный релиз с использованием аппарата Илизарова или без него, разгибательная надмыщелковая остеотомия бедренной кости, гемиэпифизеодез передней части дистальной зоны роста бедренной кости. Из многообразия методов хирургического лечения сложно выбрать наиболее эффективный, так как выполнение мягкотканных релизов достаточно часто приводит к рецидивам деформации [2, 7], остеотомии костей нельзя применять у растущих детей из-за высокого риска ремоделирования кости [8]. По данным R. Asirvatham (1993) и D.A. DelBello (1996), эффект надмыщелковой остеотомии нейтрализуется со скоростью 1° в месяц [9, 10]. Метод временного гемиэпифизеодеза является безопасным и малоинвазивным по сравнению с другими вариантами хирургического лечения [2, 4, 11–13]. Нам удалось найти лишь несколько работ, касающихся лечения пациентов со сгибательными контрактурами коленных суставов при артрогрипозе с помощью этого метода [4, 6, 12–14].
Целью исследования было оценить результаты коррекции сгибательных контрактур коленных суставов с помощью метода управляемого роста у пациентов с артрогрипозом.
Материалы и методы
В исследование было включено 12 пациентов с артрогрипозом со сгибательными контрактурами коленных суставов (20 коленных суставов), которым выполнялся временный гемиэпифизеодез передней части дистальной зоны роста бедренной кости с использованием 8-образных пластин. Соотношение мальчиков и девочек было 2 : 1. У 4 пациентов отмечалось одностороннее поражение, у 8 — двустороннее. Средний возраст на момент операции составлял 6,5 ± 0,5 года (4,3–9,6). Родители (или опекуны) всех детей добровольно подписали информированное согласие на участие в исследовании и выполнение хирургического вмешательства.
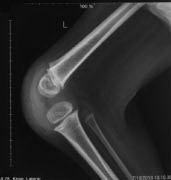
Применялся клинический и рентгенологический методы исследования. При клиническом исследовании отмечался возраст пациента на момент операции, рост, производилась оценка дефицита разгибания в коленном суставе (в градусах) и функциональной мобильности ребенка (по шкале функциональной мобильности, FMS, версия 2). Всем пациентам до и после операции выполнялись рентгенограммы коленных суставов в переднезадней и боковой проекциях.
Техника операции заключалась в супрапериостальной парапателлярной имплантации двух 8-образных пластин, каждая из которых фиксировалась двумя винтами. В процессе роста кости в части эпифизарного хряща, которая располагалась ближе к пластине, скорость роста снижалась в отличие от противоположной части, что приводило к коррекции деформации.
Возможность установки пластин определялась только размерами мыщелков бедра, а не биологическим или костным возрастом ребенка при сохраняющейся функции ростковой зоны. Пластины располагались на расстоянии 2–3 мм от медиального и латерального края надколенника, так как контакт пластины с надколенником может вызывать боль и ограничение движения в коленном суставе. Винт подбирался такой длины, чтобы его конец доходил до противоположного кортикального слоя кости, но не перфорировал его. Иммобилизация непосредственно после операции не требовалась. Пациенты продолжали пользоваться ортезами с их сменой по мере роста ребенка.
Наблюдение осуществлялось с интервалом 1 раз в 6 месяцев, оценивалась величина контрактуры и функциональная мобильность пациента. Производился расчет скорости коррекции деформации (градусы в месяц). Пластины удалялись только после полной коррекции контрактуры коленного сустава.
При обработке данных использовались статистические методы, включающие в себя оценку среднего арифметического (М), средней ошибки среднего значения (m), определение параметрического t-критерия Стьюдента. Статистическая значимость различий средних величин определялась в соответствии с таблицей критических значений t-критерия в зависимости от размера выборки. Критический уровень значимости при проверке статистических гипотез принимался равным 95 % (p ≤ 0,05). Обработку данных проводили с помощью компьютерных программ Excel 2010 и Statistica 6.0.
Результаты
Оценка эффективности применения методики временного блокирования зоны роста бедренной кости для коррекции сгибательной контрактуры коленного сустава производилась у 12 пациентов с артрогрипозом в сроки от 18 до 36 месяцев (в среднем 22,7 ± 1,08). Средняя величина дефицита разгибания коленного сустава до операции составляла 48,5 ± 4,04° (20–80°), рост пациентов (в метрах) — 1,15 ± 0,04 (0,9–1,4) (табл. 1). Контрактуры средней степени (20–50°) выявлены в 10 случаях, тяжелой (50° и более) — в 10 случаях. До начала лечения 6 пациентов не ходили, так как не могли сохранять равновесие при отсутствии поддержки, 1 пациент передвигался самостоятельно, но на небольшие расстояния, остальные 5 пациентов ходили при помощи вспомогательных средств опоры и передвижения.
Таблица 1. Возрастная характеристика пациентов и параметры контрактуры коленного сустава до и после операции
Номер пациента | Возраст на момент операции, лет. месяцев | Дефицит разгибания до операции, ° | Резидуальная деформация, ° | Период наблюдения, месяц | Скорость коррекции, градусы в месяц |
1 | 4,3 | 50 | 30 | 24 | 0,8 |
1 | 4,3 | 50 | 30 | 24 | 0,8 |
2 | 4,6 | 70 | 60 | 18 | 0,6 |
2 | 4,6 | 60 | 60 | 18 | 0 |
3 | 5,1 | 80 | 60 | 24 | 0,8 |
4 | 5,2 | 30 | 0 | 30 | 1,0 |
4 | 5,2 | 30 | 0 | 30 | 1,0 |
5 | 5,4 | 40 | 10 | 24 | 1,3 |
6 | 6,1 | 70 | 60 | 24 | 0,4 |
6 | 6,1 | 70 | 60 | 24 | 0,4 |
7 | 6,7 | 35 | 0 | 24 | 1,5 |
7 | 6,7 | 35 | 0 | 24 | 1,5 |
8 | 6,8 | 40 | 0 | 30 | 1,4 |
9 | 6,9 | 40 | 15 | 18 | 1,4 |
9 | 6,9 | 40 | 15 | 18 | 1,4 |
10 | 8,8 | 70 | 50 | 18 | 1,7 |
11 | 9,3 | 20 | 0 | 18 | 1,1 |
11 | 9,3 | 20 | 0 | 18 | 1,1 |
12 | 9,6 | 60 | 60 | 36 | 0 |
12 | 9,6 | 60 | 60 | 36 | 0 |
У 4 пациентов (№ 5, 7–9) до операции производилось консервативное устранение контрактур коленных суставов гипсовыми повязками с дистракционным устройством [15] (рис. 1). Ни у одного из них не удалось достичь полной коррекции контрактуры коленного сустава с помощью гипсовой повязки из-за появившейся боли в коленном суставе и признаков компрессии мыщелков бедра или тенденции к формированию подвывиха голени на рентгенограммах коленного сустава. Однако с помощью дополнительного метода коррекции сгибательной контрактуры произошло ее уменьшение в среднем на 38,3 ± 4,6° (20–50°), p < 0,05.






После гемиэпифизеодеза дистальной зоны роста бедренной кости было отмечено уменьшение сгибательной контрактуры коленного сустава в 17 случаях (85 %). Величина резидуальной деформации составила 28,5 ± 6,03° (0–60°). Коррекция сгибательной контрактуры за указанный период наблюдения произошла в среднем на 20° ± 2,67° (0–40°), p < 0,05.
Анализируя полученные результаты, были выявлены различия в эффективности и скорости коррекции деформации между группами пациентов с первоначальными сгибательными контрактурами менее 50° и пациентами с контрактурами 50° и более (табл. 2). У пациентов 1-й группы (10 случаев) средняя величина коррекции деформации составила 29 ± 2,1° (20–40°), что означает коррекцию на 90,1 ± 5,2 % (63–100 %). У пациентов 2-й группы (10 случаев) величина сгибательной контрактуры уменьшилась в среднем на 11 ± 2,8° (0–20°), что означает коррекцию на 47,4 ± 11,8 % (0–86 %). Различия в степени коррекции сгибательной контрактуры, выявленные в результате сравнения двух групп пациентов, были статистически значимы (t-критерий Стьюдента 3,31, p < 0,05). Закономерности в эффективности и скорости коррекции деформации у пациентов различных возрастных групп отмечено не было.
Таблица 2. Параметры контрактуры коленного сустава у пациентов сравниваемых групп
Группа пациентов | Контрактура, ° | Дефицит разгибания до операции, ° | Резидуальная деформация, ° | Величина коррекции, ° | |||
средняя | диапазон | средняя | диапазон | средняя | диапазон | ||
1-я | < 50 | 33 ± 2,5 | 20–40 | 4 ± 2,1 | 0–15 | 29 ± 2,1 | 20–40 |
2-я | 50 и > | 64 ± 3,1 | 50–80 | 53 ± 3,9 | 20–60 | 11 ± 2,8 | 0–20 |
Выявлено, что в результате лечения уровень функциональной мобильности по шкале FMS увеличился у 8 пациентов. Трое детей (№ 4, 5, 8), которые ходили при помощи вспомогательных средств передвижения, смогли от них отказаться и самостоятельно передвигаться в пределах помещения, а четверо пациентов (№ 1, 7, 9, 10), которые не ходили, стали удерживать равновесие и передвигаться с поддержкой. У одного пациента (№ 11), который самостоятельно ходил до начала лечения, увеличилась скорость и продолжительность ходьбы (на дистанции 50 и 500 метров).
В нашем исследовании было отмечено одно осложнение — миграция фиксирующего винта. Этому пациенту была снова имплантирована восьмиобразная пластина.
Обсуждение
Большинство исследователей сходятся во мнении, что использование манипуляций с ростом кости — логичный, безопасный и эффективный метод. Короткий период иммобилизации, малоинвазивность по сравнению с другими методиками, относительно простая техника операции и низкая частота осложнений — все это преимущества данного метода [2, 4, 6, 11–14, 16].
Наше исследование показало, что метод временного гемиэпифизеодеза передней части дистальной зоны роста бедренной кости позволяет уменьшить величину сгибательной контрактуры коленного сустава или устранить ее полностью, улучшив тем самым функциональную мобильность пациентов с артрогрипозом. Уменьшение сгибательной контрактуры произошло в 85 % случаев, а средняя величина коррекции составила 20 ± 2,67° (0–40°). Нам удалось получить полное разгибание в коленном суставе у трети пациентов, но даже за счет уменьшения дефицита разгибания в коленном суставе 4 пациента значительно улучшили свою функциональную мобильность (рис. 2). Во всех 8 случаях коррекция произошла в пределах 2,5 лет.







Проведенный сравнительный анализ 2-й группы пациентов с различной величиной сгибательной контрактуры коленного сустава показал, что наиболее значительно (на 90 % по сравнению с исходной величиной) происходит коррекция у пациентов с контрактурами до 50°. В этой группе были пациенты с тяжелыми сгибательными контрактурами, которым до операции производилась попытка их коррекции гипсовыми повязками с дистракционным устройством, в результате чего величина контрактуры была значительно уменьшена.
Помимо повышения эффективности лечения, применение дополнительного метода коррекции контрактуры позволяет сократить сроки лечения, что очень важно для детей с артрогрипозом. При выборе метода лечения таких пациентов всегда необходимо оценивать, могут ли функциональные ограничения, вызванные сгибательной контрактурой коленного сустава, подождать, пока происходит постепенная коррекция с помощью метода временного гемиэпифизеодеза, или требуется незамедлительная коррекция [2]. T. Palocaren, A.M. Thabet (2010) рекомендовали использовать возможности эпифизеодеза у пациентов с артрогрипозом в течение 3 лет, а затем, если контрактура коленного сустава влияет на способность передвигаться, применять другие методы хирургического лечения [14].
Все это говорит о необходимости в случае тяжелых контрактур коленных суставов использовать дополнительные методы коррекции контрактур, чтобы перевести их в средние и легкие, и только затем применять метод гемиэпифизеодеза. С этой же целью J. Klatt и P.M. Stevens рекомендовали сочетать операцию временного эпифизеодеза с рецессией сгибателей голени [12].
В связи с тем что в исследование было включено небольшое количество пациентов и период наблюдения был коротким, для более достоверной оценки результатов лечения детей разных возрастных групп с различной степенью контрактуры в дальнейшем потребуется проведение большого проспективного исследования.
Выводы
Метод временного гемиэпифизеодеза является эффективным, безопасным и менее инвазивным по сравнению с другими методиками и может применяться для лечения детей с артрогрипозом.
Сочетание гемиэпифизеодеза с дополнительными методами коррекции сгибательной контрактуры помогает значительно уменьшить ее величину, переводя ее из тяжелой в умеренную, делая тем самым лечение более эффективным и менее продолжительным, что позволяет в кратчайшие сроки достичь вертикализации пациента.
Информация о финансировании и конфликте интересов
Работа проведена на базе и при поддержке ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России. Авторы декларируют отсутствие явных и потенциальных конфликтов интересов, связанных с публикацией настоящей статьи.
Об авторах
Светлана Ивановна Трофимова
ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
Автор, ответственный за переписку.
Email: trofimova_sv2012@mail.ru
канд. мед. наук, научный сотрудник отделения артрогрипоза Россия
Дмитрий Степанович Буклаев
ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
Email: fake@eco-vector.ru
канд. мед. наук, заведующий отделением артрогрипоза Россия
Екатерина Владимировна Петрова
ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
Email: fake@eco-vector.ru
канд. мед. наук, старший научный сотрудник отделения артрогрипоза Россия
Светлана Александровна Мулеванова
ФГБУ «НИДОИ им. Г.И. Турнера» Минздрава России
Email: fake@eco-vector.ru
аспирант отделения артрогрипоза Россия
Список литературы
- Лапкин Ю.А., Конюхов М.П. Лечение наиболее распространенных деформаций нижних конечностей при артрогрипозе // Травматология и ортопедия России. — 2002. — № 3. — С. 86–92. [Lapkin YuA, Konyukhov MP. Lechenie naibolee rasprostranennykh deformatsii nizhnikh konechnostei pri artrogripoze. Travmatologiya i ortopediya Rossii. 2002;(3):86-92. (In Russ.)]
- Lampasi M, Antonioli D, Donzelli O. Management of knee deformities in children with arthrogryposis. Musculoskelet Surg. 2012;96(3):161-169. doi: 10.1007/s12306-012-0218-z.
- Murray C, Fixsen JA. Management of knee deformity in classical arthrogryposis multiplex congenita (amyoplasia congenita). J Pediatr Orthop B. 1997;6(3):186-191. doi: 10.1097/01202412-199707000-00006.
- MacWilliams BA, Harjinder B, Stevens PM. Guided growth for correction of knee flexion deformity: a series of four cases. Strat Traum Limb Recon. 2011;6:83-90. doi: 10.1007/s11751-011-0110-7.
- Mielke CH, Stevens PM. Hemiepiphyseal stapling for knee deformities in children younger than 10 years. J Pediatr Orthop. 1996;16:423-429. doi: 10.1097/01241398-199607000-00002.
- Al-Aubaidi Z, Lundgaard B, Pedersen NW. Anterior distal femoral hemiepiphysiodesis in the treatment of fixed knee flexion contracture in neuromuscular patients. J Child Orthop. 2012;6(4):313-318. doi: 10.1007/s11832-012-0415-1.
- van Bosse HJ, Feldman DS, Anavian J, Sala DA. Treatment of knee flexion contractures in patients with arthrogryposis. J Pediatr Orthop. 2007;27(8):930-937. doi: 10.1097/bpo.0b013e3181594cd0.
- Moreira MV, Rimoldi AC, Aoki S. Analysis on the results from percutaneous extensor osteotomy of the distal femur in patients with amyoplasia. Rev Bras Ortop. 2014;49(4):345-349. doi: 10.1016/j.rboe.2014.04.017.
- Asirvatham R, Mukherjee A, Agarwal S, et al. Supracondylar femoral extension osteotomy. J Pediatr Orthop. 1993;13(5):642-645. doi: 10.1097/01241398-199313050-00016.
- DelBello DA, Watts HG. Distal femoral extension osteotomy for knee flexion contracture in patients with arthrogryposis. J Pediatr Orthop. 1996;16:122-126. doi: 10.1097/01241398-199601000-00025.
- Eastwood DM, Sanghrajka AP. Guided growth recent advances in a deep-rooted concept. J Bone Joint Surg. 2011;93(B):12-18. doi: 10.1302/0301-620X.93B1.25181.
- Klatt J, Stevens PM. Guided growth for fixed knee flexion deformity. J Pediatr Orthop. 2008;28:626-631. doi: 10.1097/BPO.0b013e318183d573.
- Kramer A, Stevens PM. Anterior femoral stapling. J Pediatr Orthop. 2001;21(6):804-807. doi: 10.1097/01241398-200111000-00020.
- Palocaren T, Thabet AM, Rogers K, et al. Anterior distal femoral stapling for correcting knee flexion contracture in children with arthrogryposis-preliminary results. J Pediatr Orthop. 2010;30(2):169-173. doi: 10.1097/BPO.0b013e3181d07593.
- Агранович О.Е., Баиндурашвили А.Г., Петрова Е.В., и др. Консервативное лечение деформаций верхних и нижних конечностей у детей раннего возраста с артрогрипозом // Детская хирургия. — 2012. — № 2. — С. 10–15. [Agranovich OE, Baindurashvili AG, Petrova EV, et al. Konservativnoe lechenie deformatsii verkhnikh i nizhnikh konechnostei u detei rannego vozrasta s artrogripozom. Detskaya khirurgiya. 2012;(2):10-15. (In Russ.)]
- Кенис. В.М., Клычкова И.Ю., Мельченко Е.В., и др. Коррекция деформаций нижних конечностей у детей с помощью метода управляемого роста // Вестник травматологии и ортопедии им. Н.Н. Приорова. — 2013. — № 4. — С. 50–55. [Kenis VM, Klychkova IY, Melchenko EV, et al. Guided growth technique for correction of lower extremity deformities in children. Vestnik travmatologii i ortopedii im N.N. Priorova. 2013;(4):50-55. (In Russ.)]
Дополнительные файлы