Clinical forms of shoulder instability in pediatric patients
- 作者: Proshchenko Y.N.1, Baindurashvili A.G.1, Brianskaia A.I.1, Prokopovich E.V.1, Nikitin M.S.1, Afonichev K.A.1
-
隶属关系:
- The Turner Scientific and Research Institute for Children’s Orthopedics
- 期: 卷 4, 编号 4 (2016)
- 页面: 41-46
- 栏目: Articles
- ##submission.dateSubmitted##: 09.01.2017
- ##submission.dateAccepted##: 09.01.2017
- ##submission.datePublished##: 14.12.2016
- URL: https://journals.eco-vector.com/turner/article/view/5894
- DOI: https://doi.org/10.17816/PTORS4441-46
- ID: 5894
如何引用文章
详细
Background. The recurrence rate of adolescent chronic shoulder instability is approximately 56%–68%. However, this pathology is often missed in childhood and adolescence.
Aim. To identify the clinical forms of shoulder joint instability in pediatric patients.
Materials and methods. The authors present the data from 57 pediatric patients aged 3−17 years with a total of 61 unstable shoulder joints. All patients were divided into groups according to the form of instability. Traumatic chronic shoulder instability was identified in 40 patients (Bankart and Hill–Sachs injuries). Of these, non-traumatic shoulder instability was diagnose in 17, including five with recurrent dislocation, and spontaneous shoulder dislocation due to dysplasia of glenoid and labrum was diagnosed in 12. Of the 57 patients in the study cohort, 53 underwent surgery. Postoperatively, two patients developed recurrent shoulder dislocation (Andreev–Boichev technique) due type III shoulder dysplasia in the first patient and multidirectional injury in the second.
Conclusions. Shoulder joint instability should be considered as the traumatic or non-traumatic form. Treatment decisions should be based on anatomical characteristics that predispose to recurrent dislocation.
关键词
全文:
Background
Shoulder joint instability is a pathological condition characterized by a defect in proper centering of the humeral head in the glenoid cavity of the scapula. This occurs due to failure of the surrounding stabilizing structures of the joint [1, 2]. Overall, shoulder instability is common in children [3, 4].
Chronic instability of the shoulder joint occurs to varying degrees [5], and can lead to the development of habitual shoulder dislocation, which is seen in 56%–68% of young patients. [6] However, though there are several publications on the classification, treatment, and diagnosis of shoulder instability in adults [7, 8], there are few publications devoted to this problem in children [9, 10].
Aim: To address clinical forms of shoulder joint instability in children.
Clinical population We evaluated 57 children aged from 3 to 17 years with 61 unstable shoulder joints (40 males, 17 females).
Methods: Clinical, X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) data were evaluated. For statistical analysis, we used the set of standard analysis tools included in Statistica 6.0. All patients signed a voluntary informed consent form for participation in the study and for surgery.
Introduction
Currently, orthopedists do not have a classification system for shoulder joint instability in pediatric patients that adequately addresses the form, nature, or type of instability in the shoulder joint. Therefore, we grouped the features of instability that are already understood into a single classification system, centered around the main features of instability (Table 1).
Table 1. Classification of shoulder joint instability in children
Shoulder joint instability with an indication of the affected side (right, left) | |||
Form of instability | Characteristics of instability (dislocation) | Type and direction of displacement | Instability degree |
Traumatic | Habitual | Anterior or posterior Upward or downward Multidirectional | Decentration |
Atraumatic | Habitual Arbitrary | Subluxation | |
Dislocation | |||
Instability of the shoulder joint: Traumatic form (70.2%, n = 40/57)
Diagnosis. Habitual shoulder dislocation (100%, n = 40/57).
In the group with habitual shoulder dislocation, the age range of the patients was 14–17 years old. The right shoulder joint was unstable in 28 patients, while the left shoulder joint was unstable in 12 patients. Anteroinferior displacement was observed in 38 patients, posterosuperior displacement was observed in 1 patient, and multidirectional displacement was observed in 1 patient.
During the clinical examination, the degree of translation was measured [11] and 2nd and 3rd degree translation was observed in affected joints. Two radiological examinations were performed, to determine anatomical type (shape and size ratio), epiphyseal-diaphyseal angle, and the glenoid inclination angle. A CT examination was also performed, which allowed detection of a type 3 ratio of the head and articular process in one patient (Fig. 1), as well as one case of retroversion of the humeral head. In 10 patients, a Bankart type fracture of the articular process was observed.
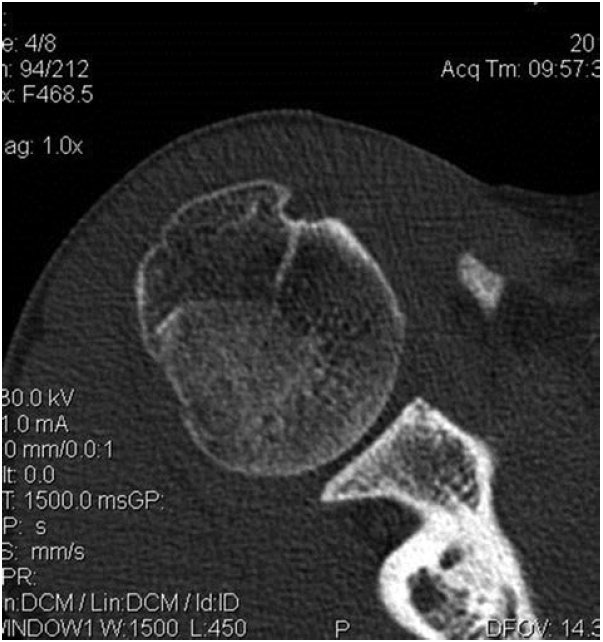
Fig. 1. Patient M., 15 years old. Right shoulder joint instability, traumatic form. Habitual anteroinferior dislocation. Type 3 ratio of the right humeral head and the scapula articular process. Length of the articular surface is reduced (the head is bigger than the scapula articular surface)
In order to determine the extent of damage to the stabilizing shoulder joint structures, we performed MRI on the patients. In 28 patients, damage to the fibrous lip was diagnosed, and in 14 patients a Hill–Sachs defect and Bankart lesion were diagnosed.
In total, in 38 patients a traumatic pathology was diagnosed (the Hill–Sachs defect and the Bankart lesion), including 10 children with a Bankart fracture of the articular process. Two patients had an anatomical predisposition to the injury (type 3 ratio, retroversion of 10 degrees). Additionally, we found that the degree of translation and the severity of anatomic lesions is correlated, and that 2–3 degrees of translation can indicate more severe traumatic injury.
Surgical treatment
Arthroscopy was performed in 35 patients, and in 26 patients of these patients arthroscopic stabilization was performed (stay sutures of the front lip and remplissage of the supraspinous muscle for the head defect).
Isolated tenodesis of the biceps long head was performed in 1 patient (isolated transposition of the biceps long head posterior to the greater tubercle). This type of transposition is used for retroversion correction.
Joint capsule grafting, front lip sutures, and transposition of the biceps long head was performed in 1 patient (11 year-old female). Her medical history included a dislocation-fracture, multiple repositioning, and failure to meet the time limit for immobilization. A Bankart lesion and dislocation of the biceps long head was found intraoperatively.
Muscular surgery was performed in 2 patients (method developed by Andreev–Boychev). Finally, transposition of the coracoid process was performed in 10 patients.
Surgical Results. One year after surgery, a patient that underwent the Andreev-Boychev surgery had a relapse of the anteroinferior dislocation during athletic activity. Additionally, a patient that underwent arthroscopic stabilization had a recurrence 9 months after the surgery during a physical education lesson.
Instability of the shoulder joint: Atraumatic form (29.8%, n = 17/57)
Diagnostics. Dysplastic habitual shoulder dislocation (17.6%, n = 3/17).
These patients all had dysplastic shoulder dislocation due to congenital malformation of the cervical spine, known as Klippel–Feil syndrome. Their examination included a comparative X-ray (Fig. 2) and a CT scan, which evaluated the inclination angle and rotation angle of the glenoid and the articular process area. These examinations revealed excessive glenoid inclination in these patients that was due to dysplasia of the scapula articular process.
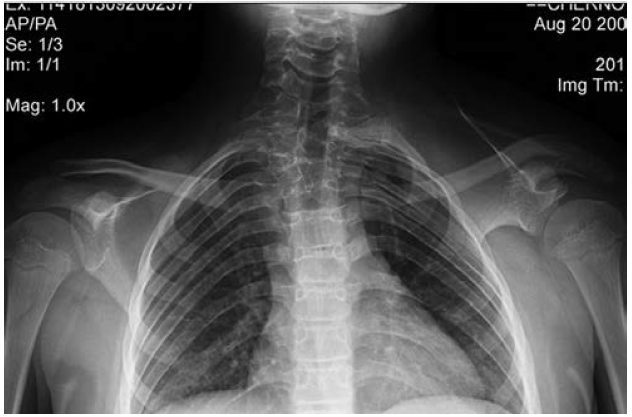
Fig. 2. Instability of the left shoulder joint, atraumatic form. Habitual multidirectional subluxation. Dysplasia of the scapula articular process on the left, subluxation of the left shoulder head
Method of treatment: The injuries were treated conservatively, and were aimed at strengthening the shoulder muscles.
Diagnostics. Habitual shoulder dislocation (11.7%, n = 2/17).
Two patients were included in this category: a 15 year-old female that had a multidirectional left-sided dislocation, and a 16 year-old male with habitual anteroinferior dislocation. Their injury histories were not well described. Clinical instability was detected in both joints.
The examinations included X-ray and CT studies of the shoulder joint. The CT revealed that the 15 year-old patient had retroversion of the left humeral head (Fig. 3). Additionally, MRI and electroneuromyography examinations by a neurologist were performed, but did not reveal anything further regarding the pathology.
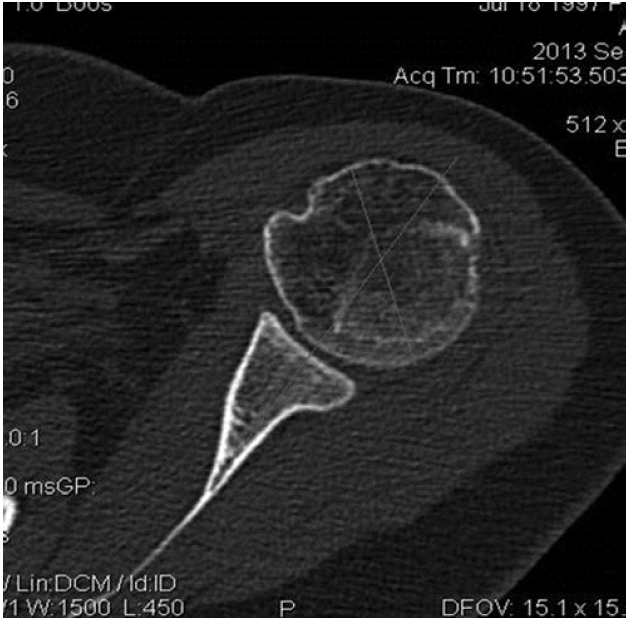
Fig. 3. Patient D., 15 years old. Instability of the left shoulder joint, combined form. Habitual multidirectional subluxation. Retroversion of the left humeral head
Method of treatment. Arthroscopy of the left shoulder revealed an increased volume in the lower parts of the left shoulder joint. Capsulorrhaphy of the lower parts of the left shoulder joint was performed, followed by corrective osteotomy of the shoulder.
Surgical Results. The patients were examined 6 months after surgery. 1st degree instability remained (as per S. Lintner). X-ray examination indicated that the downward subluxation was eliminated.
Diagnostics. Arbitrary shoulder dislocation (70.7%, n = 12/17, 18 joints total).
In this group, the right and left shoulder joint were affected at the same rate. A bilateral lesion was found in four patients. Only a 12-year-old female with bilateral arbitrary dislocation did not complain of pain and discomfort during the dislocation.
Examination included two comparative radiological exams, CT, MRI, and an evaluation by a neurologist. No diagnostically significant changes were found. In cases of arbitrary dislocation, previous studies indicate that this type of injury typically occurs in children 5–7 years of age [12] and is characterized by the absence of any anatomical changes in the shoulder joint [13]. Rowe (1973) reported that electromyographic examination revealed no shoulder joint muscle pathology in 26 children with arbitrary shoulder dislocation [14]. Similarly, Patralekh (2012) performed CT studies of the shoulder joint with 3D-reconstruction and found no bone diseases [15]. Additionally, Leftor et al. (2004) examined 29 patients aged from 5 to 15 years, 15 of which had posterior dislocation, 4 anterior dislocation, and 10 multidirectional instability [16]. This group found no anatomical changes in the patients, only traumatic defects of humeral head cartilage in two patients, which was due to continued trauma from dislocation.
Arthroscopy of the shoulder joint and the glenoid lip dysplasia was performed in 8 cases of unilateral lesions (Fig. 4). The cause of instability in these cases appears to be dysplasia of the fibrous lip of the scapular articular process.
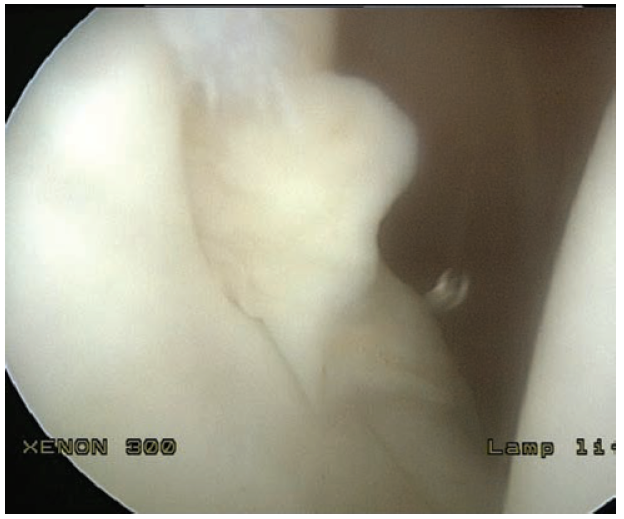
Fig. 4. Patient M, 15 years old. Right shoulder joint instability, atraumatic form. Arbitrary posterosuperior dislocation. Arthroscopic photo of the dysplastic posterior lip of the right shoulder joint
Method of treatment: In one patient with a bilateral lesion (12 year-old female), surgical treatment was not performed. Instead, conservative therapy was pursued. In one male with a bilateral lesion, the Andreev–Boychev surgery was performed on his right shoulder. In 12 cases arthroscopic stabilization was performed (stay sutures of the lip).
Surgical results. Of the 13 shoulder joint surgeries performed (n = 13), no repeat dislocations were observed.
Discussion
We analyzed shoulder joint instability in children and determined a classification system based on the form, type, direction, and extent of displacement of the humeral head. This combines previously disaggregated data into a single etiopathogenic chain, which will be convenient for future clinical practice. In our classification of shoulder joint instability, we include an atraumatic form, which can be caused by a number of factors. The diagnostically relevant methods of examination in our study were X-ray, CT, MRI, and arthroscopy. Using these methods the anatomical changes in bone structures can be determined (extent and type of displacement, anatomical type, and retroversion), and the presence of lesions or dysplasia of soft tissue intra-articular structures of the shoulder joint can be established reliably.
Glazunova (2003) reported that a significant percentage of all cases of disorders of the shoulder joint may follow a neonatal dislocation or subluxation [17]. Reading (2012) suggested that many of these are misdiagnosed as dysplastic, and instead they may be primarily neurogenic with subsequent development of dysplastic changes in the shoulder joints [18]. Previous descriptions of congenital dislocation of the shoulder have also been made. For example, Sudesh (2010) [19] reviewed the classification of congenital shoulder dislocation proposed by Whitman (1905) [20], and suggests that there are secondary dislocations resulting from birth injury. This supports the introduction of an atraumatic classification of shoulder joint instability, and reflects a combination of many factors that contribute to shoulder instability in children.
The surgery was performed in 53 patients (53 joints), and shoulder dislocation re-occurred in 2 patients (2 joints). Patients with dysplasia of the scapula articular process is the most problematic for surgical treatment, as there are no reliable data regarding which surgery should be performed and when it should be done to best stabilize the shoulder. In the first case that dislocation recurred, the patient had a type 3 ratio of the humeral head and articular process. Transposition of the coracoid process on the anterior part of the articular process was performed in this patient. We believed that growth would promote self-correction in the joint and that this would strengthen the anterior part of the joint capsule. The second case of dislocation recurrence occurred in a patient that had multidirectional dislocation. We performed arthroscopic stabilization in this patient and repeated surgery was required.
Conclusions
In children, shoulder instability can be categorized into traumatic and atraumatic forms. Children with shoulder instability in the absence of shoulder pathology likely require arthroscopic approaches. When choosing a surgical treatment, methods aimed at elimination of the anatomical cause of instability that are also likely to prevent the recurrence of dislocation should be selected, if possible.
Funding and Conflict of Interest
This work was performed with the support of The Turner Scientific and Research institute for Children’s Orthopedics. The authors declare no conflicts of interest associated with the publication of this article.
作者简介
Yaroslav Proshchenko
The Turner Scientific and Research Institute for Children’s Orthopedics
编辑信件的主要联系方式.
Email: Yar2011@list.ru
MD, PhD, research associate of the department of trauma effects and rheumatoid arthritis 俄罗斯联邦
Alexei Baindurashvili
The Turner Scientific and Research Institute for Children’s Orthopedics
Email: turner01@mail.ru
MD, PhD, professor, member of RAS, honored doctor of the Russian Federation, Director of The Turner Scientific and Research Institute for Children’s Orthopedics 俄罗斯联邦
Ananstasiya Brianskaia
The Turner Scientific and Research Institute for Children’s Orthopedics
Email: a_bryanskaya@mail.ru
MD, PhD, research associate of the department of trauma effects and rheumatoid arthritis 俄罗斯联邦
Evgeny Prokopovich
The Turner Scientific and Research Institute for Children’s Orthopedics
Email: fake@eco-vector.ru
MD, PhD, orthopedic surgeon of the department of trauma sequelae and rheumatoid arthritis 俄罗斯联邦
Maksim Nikitin
The Turner Scientific and Research Institute for Children’s Orthopedics
Email: fake@eco-vector.ru
MD, orthopedic and trauma surgeon of the department of trauma effects and rheumatoid arthritis 俄罗斯联邦
Konstantin Afonichev
The Turner Scientific and Research Institute for Children’s Orthopedics
Email: afonichev@list.ru
MD, PhD, professor, head of the department of trauma effects and rheumatoid arthritis 俄罗斯联邦
参考
- Длясин Н.Г., Норкин А.И., Грамма С.А., и др. Современные методы лечения привычного вывиха плеча (обзор литературы) // Саратовский научно-медицинский журнал. — 2010. — Т. 6. — № 3. — С. 687–692. [Dlyasin NG, Norkin AI, Gramma SA, et al. Modern Treatment Methods of Habitual Shoulder Dislocation (Literature Review). Saratov Journal of Medical Scientific Research. 2010;6(3):687-692. (In Russ.)]
- Мицкевич В.А. Нестабильность плечевого сустава // Consilium Medicum. — 2004. — Т. 6. — № 2. — С. 87–92. [Mickevich VA. Nestabil’nost’ plechevogo sustava. Consilium Medicum. 2004;6(2):87-92. (In Russ.)]
- Isik M, Subasi M, Cebesoy O, et al. Traumatic shoulder fracture-dislocation in a 7-year-old child: a case report. J Med Case Rep. 2013;7(1):156. doi: 10.1186/1752-1947-7-156.
- Kraus R, Pavlidis T, Dongowski N, et al. Children and adolescents with posttraumatic shoulder instability benefit from arthroscopic stabilization. Eur J Pediatr Surg. 2010;20(4):253-6. doi: 10.1055/s-0030-1252004.
- Blum A, Coudane Н, Molé D. Gleno-humeral instabilities. Eur Radiol. 2000;10(1):63-82. doi: 10.1007/s003300050008.
- Robinson MC. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. The Journal of Bone and Joint Surgery (American). 2006:88(11):2326. doi: 10.2106/jbjs.e.01327.
- Доколин С.Ю. Хирургическое лечение больных с передними вывихами плеча с использованием артроскопии: клинико-экспериментальное исследование: Дис. … канд. мед. наук. — СПб., 2002. — 151 с. [Dokolin SY. Surgical treatment of patients with forward dislocations of a shoulder with arthroscopy use: kliniko-experiment study. [dissertation]. Saint Peterburg; 2002. (In Russ.)]
- Тяжелов А.А. Классификация нестабильности плечевого сустава // Вестн. травматол. и ортопед. им. Н.Н. Приорова. — 1999. — № 4. — С. 13–17. [Tyazhelov AA. Classification of instability of a humeral joint. Vestn. travmatol. i ortoped. im. N.N. Priorova. 1999;(4):13-17. (In Russ.)]
- Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl. 2009;91(1):2-7. doi: 10.1308/003588409x359123.
- Cordischi K, Li X, Busconi B. Intermediate outcomes after primary traumatic anterior shoulder dislocation in skeletally immature patients aged 10 to 13 years. Orthopedics. 2009;32(9):686-690. doi: 10.3928/01477447-20090728-34.
- Lintner S. Glenohumeral Translation in the Asymptomatic Athlete's Shoulder and Its Relationship to Other Clinically Measurable Anthropometric Variables. Am J Sports Med. 1996;24(6):716-21. doi: 10.1177/036354659602400603.
- Papavasileiou A, Kitsis C. Multidirectional voluntary glenohumeral dislocation in a 7-year-old patient: a case report. Acta Orthopaedica Belgica. 2003;69(6):558-561.
- Neer CS, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder: a preliminary report. J Bone Joint Surg. 1980;62-A:897-908.
- Rowe CR, Pierce DS, Clark JG. Voluntary dislocation of the shoulder: a preliminary report on a clinical, electromyographic, and psychiatric study of twenty-six patients. J Bone Joint Surg Am. 1973;55:445-460.
- Patralekh MK, Maini L, Kalra M. Voluntary anterior dislocation of the shoulder in a 10-year-old child treated surgically. J Hand Microsurg. 2012;4(1):32-33. doi: 10.1007/s12593-011-0057-4.
- Leftor G, Pfliger F, Mal-Lawane M. Capsular shift for voluntary dislocation of the shoulder: results in children. Rev Chir Orthop Reparatrice Appar Mot. 2004;90(7):607-612.
- Глазунова Н.Ю. Нейрогенные аспекты дисплазии плечевых суставов у детей раннего возраста (клиника, патогенез, лечение): Дис. … канд. мед. наук. — М., 2003. — 121 с. [Glazunovа NY. Neurogenetic aspects of a displaziya of humeral joints at children of early age (clinic, pathogenesis, treatment). [dissertation] Moscow; 2003. (In Russ.)]
- Reading BD, Laor T, Salisbury SR, et al. Quantification of humeral head deformity following neonatal brachial plexus palsy. J Bone Joint Surg Am. 2012;94(18):e136-1. doi: 10.2106/jbjs.k.00540.
- Sudesh P, Rangdal S, Bali K. True congenital dislocation of shoulder: A case report and review of the literature. Int J Shoulder Surg. 2010;4(4):102. doi: 10.4103/0973-6042.79798.
- Whitman R. The treatment of congenital and acquired luxations at the shoulder in childhood. Ann Surg. 1905;42(1):110-115. doi: 10.1097/00000658-190507000-00008.
补充文件