Развитие общей врачебной практики / семейной медицины в Санкт-Петербурге (Российская Федерация)
- Авторы: Гиллан У.1, Маккуистон Р.1, Слевин О.1
-
Учреждения:
- Группа исследования и развития здравоохранения*, Ольстерский университет
- Выпуск: Том 23, № 4 (2019)
- Страницы: 19-31
- Раздел: Теория и практика
- Статья получена: 23.12.2019
- Статья одобрена: 10.01.2020
- Статья опубликована: 11.02.2020
- URL: https://journals.eco-vector.com/RFD/article/view/18921
- DOI: https://doi.org/10.17816/RFD18921
- ID: 18921
Цитировать
Аннотация
В предшествующие годы в Российской Федерации большое внимание уделялось разработке новых подходов к общей врачебной практике. Особое внимание было сосредоточено на создании системы общей врачебной практики (семейной медицины) и подготовке семейных врачей. Был проведен ряд пилотных исследований, в том числе в Санкт-Петербурге. Эти исследования были направлены на обеспечение условий для тестирования и развития новых, более эффективных подходов к первичной медико-санитарной помощи, которые лучше интегрируются с другими видами медицинской помощи. Авторы участвовали в начальном пилотном исследовании в середине и конце 1990-х гг. и в последующих проектах по дальнейшему развитию системы общей врачебной практики в 2002–2010 гг. В данной статье представлены результаты, достигнутые при решении вышеупомянутых задач. Авторы не дают полную комплексную оценку всей системы здравоохранения в ее современном виде, тем не менее представленные данные свидетельствуют о прогрессе в целом ряде направлений практической деятельности. В обзоре рассмотрены проблемы, возникшие при реализации новых подходов, а также предложения, которые могут быть полезными для стратегического планирования развития здравоохранения.
Полный текст
Введение: начало, вызовы и новые направления
Начало. В XX в. Советский Союз, а позже — Российская Федерация, продолжали прогрессивно развиваться в соответствии с тенденциями современности. Как и везде модернизация промышленности в России происходила благодаря научно-техническому прогрессу, присущему новой постиндустриальной эпохе. Эти события также повлияли на вопросы охраны здоровья и благополучия. Были достигнуты успехи в профилактике, диагностике и лечении «старых» заболеваний, таких как полиомиелит, туберкулез, корь, дифтерия и брюшной тиф. Однако появились новые проблемы, связанные с распространением неинфекционных хронических заболеваний, во многом обусловленных поведенческими факторами риска. В некоторой степени они вытеснили инфекционные болезни. Сердечно-сосудистые заболевания, ожирение, диабет, бронхиальная астма и другие респираторные заболевания (часто связанные с курением и промышленным загрязнением), некоторые злокачественные заболевания, алкоголизм и злоупотребление наркотиками, а также проблемы с психическим здоровьем — всех этих проблем стало больше. Ожидания современности — что утопические идеи о полном здоровье и благополучии сбудутся — были в некоторой степени заменены постмодернистским страхом в отношении возникающих проблем со здоровьем.
Вызовы. Во второй половине XX столетия количество эпидемий, приводивших к масштабной гибели населения, сократилось, утихли мировые конфликты и был ликвидирован голод (по крайней мере, в развитых странах). Значительные изменения также произошли в области гигиены окружающей среды (например, чистая вода, канализация, утилизация отходов и гигиена пищевых продуктов). Это оказало значительное положительное влияние на общее состояние здоровья и благосостояние населения на Западе и в других развитых странах и привело к сопутствующим изменениям в плане увеличения численности населения и изменения общих демографических характеристик. По мере снижения младенческой и общей смертности продолжительность жизни увеличивалась, что привело к увеличению доли пожилых и старых людей. Эти тенденции обусловливают повышенные требования к службам здравоохранения и социального обеспечения. В значительной степени эти тенденции отмечались и в Российской Федерации, хотя и с некоторыми существенными отклонениями. Как показано на рис. 1, со времени Великой Отечественной войны (Вторая мировая война) до 1991 г., непосредственно перед распадом СССР и созданием Российской Федерации, коэффициенты младенческой смертности (infant mortality rate — IMR) в значительной степени имели тенденцию к снижению [1].
Рис. 1. Частота младенческой смертности: СССР и Российская Федерация [1]
Хотя приведенный выше показатель является хорошим индикатором позитивных тенденций в области здравоохранения, важно также признать уникальную ситуацию, которая имеет место в России. Конечно, у всех стран свои уникальные особенности в отношении населения и демографии, культуры, физической среды и т. д. Однако Россия является самой большой страной в мире по занимаемой территории. Она простирается от Арктики до юга Центральной Азии, через Европу и Азию — общая площадь страны составляет около 6,7 млн км2. Это 9-я страна с наибольшим населением на Земле, составляющим около 145 млн человек. При этом бóльшая часть населения проживает в европейской части страны, что объясняется неблагоприятным климатом и географической отдаленностью значительной части территории.
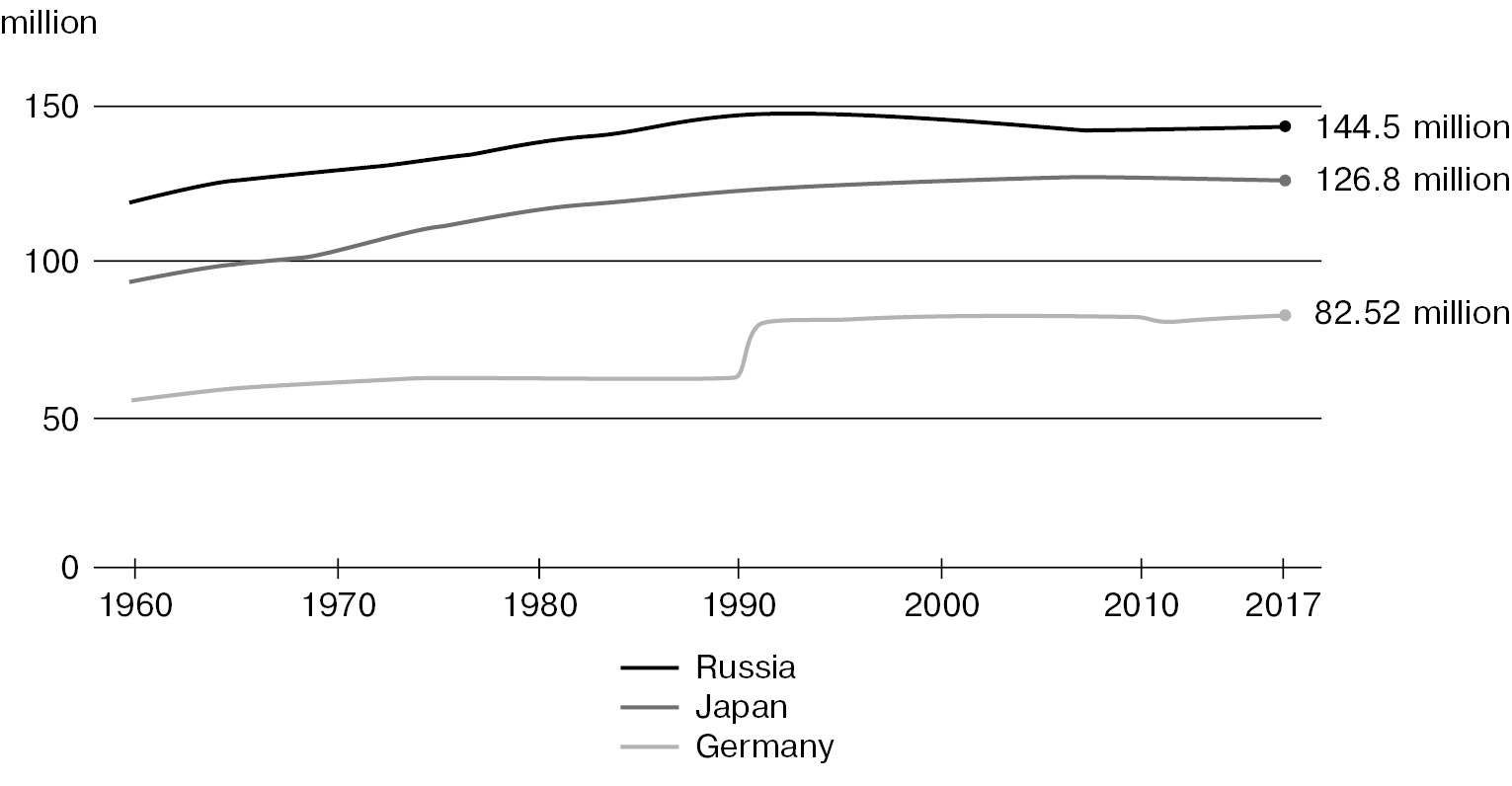
Оценка, с учетом приведенных данных за период с 1960 по 2017 гг., показала, что в 2019 г. численность населения России составляет 145,87 млн человек, что ниже по сравнению с расчетными предполагаемыми показателями от 2015 г., составляющими 146,3 млн человек [2]. Таким образом, Россия не полностью повторяет тенденции других развитых стран, являясь одной из очень немногих, где за последние два-три десятилетия наблюдался отрицательный прирост населения. Как видно из рис. 2 [3], в то время как другие развитые страны, например Германия и Япония (также сильно пострадавшие от Второй мировой войны), имели устойчивый рост численности населения и увеличение ожидаемой продолжительности жизни, в России ситуация была иной: в последнее время отмечались не только тенденции к снижению общей численности населения, но и снижение миграции, особенно в отношении внутренней иммиграции [4].
Рис. 2. Рост численности населения России, Японии и Германии (1960–2017) [3]
В России отмечается низкий уровень рождаемости в сочетании с высоким уровнем абортов. Это может быть связано с экономическим спадом и нежеланием производить потомство при не слишком благоприятных обстоятельствах. Предполагается, что в СССР существовала тенденция, распространяющаяся на нынешнюю Российскую Федерацию, в результате которой аборт использовался и продолжает использоваться многими женщинами в качестве средства контроля рождаемости [5]. Это привело к растущей обеспокоенности и стремлению правительства выработать стратегии по сокращению числа абортов. Проблема низкой рождаемости и сокращения численности населения усугубляется и другими факторами, например высоким уровнем смертности среди молодых людей, в частности мужчин, что связано с употреблением алкоголя, самоубийствами, несчастными случаями и насильственными причинами (количество убийств в этой группе больше только в Колумбии и некоторых частях Мексики и США). В этом отношении следует отметить, что предыдущая правительственная кампания по борьбе с разрушительным воздействием алкоголизма, начатая до крупных социальных изменений при распаде СССР, действительно оказала заметное положительное влияние на уровень смертности и продолжительность жизни в течение определенного периода. Однако сложившаяся политическая ситуация не позволила продолжить эту кампанию.
В то время, когда проводились пилотные исследования, рассматриваемые в данной статье, ранние этапы социально-политической трансформации СССР не были достаточно проработаны, чтобы более четко продемонстрировать тенденции развития системы здравоохранения. Тем не менее, как уже было признано политическими лидерами, в этой системе были необходимы изменения. Это становится все более очевидным, исходя из основных показателей здоровья, таких как данные об ожидаемой продолжительности жизни (табл. 1) [1], а также из оценок и представлений медицинских работников. Ранее существовавшие идеалистические патерналистские системы здравоохранения не соответствовали возникшим перед ними задачам и вызовам [6]. Таким образом, можно предположить, что Россия уникальна во многих отношениях. В связи с этим, несмотря на то что важно учитывать развитие здравоохранения в целом и в глобальном масштабе, а также лучшие практики и опыт других стран, также крайне важно, чтобы они рассматривались с учетом особенностей России.
Таблица 1
Ожидаемая продолжительность жизни (годы) [1]
Годы | Россия | США | ||||
Мужчины | Женщины | Разница | Мужчины | Женщины | Разница | |
1896 | 30,9 | 33,0 | 2,1 | – | – | – |
1910 | – | – | – | 48,4 | 51,8 | 3,4 |
1926 | 39,3 | 44,8 | 5,5 | 55,5 | 58,0 | 2,5 |
1938 | 40,4 | 46,7 | 6,3 | 61,9 | 65,3 | 3,4 |
1958 | 61,9 | 69,2 | 7,3 | 66,8 | 73,2 | 6,4 |
1965 | 64,0 | 72,1 | 8,1 | 66,9 | 73,7 | 6,8 |
1970 | 63,0 | 73,4 | 10,4 | 67,1 | 74,7 | 7,6 |
1980 | 61,4 | 73,0 | 11,6 | 70,0 | 77,4 | 7,4 |
1987 | 64,9 | 74,3 | 9,4 | 71,5 | 78,4 | 6,9 |
1990 | 63,8 | 74,4 | 10,6 | 72,0 | 78,8 | 6,8 |
1991 | 63,5 | 74,3 | 10,8 | 72,0 | 78,9 | 6,9 |
Различия между российской системой и системами медицинского обеспечения некоторых западных стран отмечались неоднократно. Также были отмечены различия в фактических угрозах здоровью и в том, как бремя этих угроз ложится на мужчин, особенно на молодых, как это было определено В. Школьниковым и С. Месле [1], Б.А. Розенфельдом [6] и другими авторами.
П. Тун писал, что российская система здравоохранения также отличается от многих других развитых стран исключительной обширностью [7]. Он отмечал, что медицинские услуги по сравнению с другими странами могут быть лучше или хуже, а могут быть просто другими. П. Тун и др. также писали, что перед Россией стояли не только вызовы, связанные с оказанием медицинской помощи, с которыми сталкивается большинство развитых стран, но и другие специфические российские обстоятельства [7]. Они включали уже упомянутые конкретные демографические и эпидемиологические проблемы (низкий уровень рождаемости, высокий уровень абортов, высокий уровень алкоголизма, особенно среди молодежи, более низкие экономические показатели и исключительно низкий уровень иммиграции).
Новые направления. Развитие общей врачебной практики / семейной медицины (ОВП/СМ) в Санкт-Петербурге с проведением пилотных исследований происходило в период серьезных перемен в России. Первоначальные проекты первичной медико-санитарной помощи TACIS (Technical Assistance for the Commonwealth of Independent States, Техническая помощь Содружеству Независимых Государств) были задуманы в 1993–1994 гг. и осуществлялись с 1995 по 1998 г. С 2002 по 2005 г. были продолжены работы по развитию первичной медико-санитарной помощи (ПМСП) в Москве и Белгороде, а в 2006–2010 гг. — по улучшению состояния здоровья населения Калининградской области. Незадолго до начала разработки первых проектов в начале 1990-х гг. в России произошли серьезные изменения. Их можно назвать столь же революционными, как и распад царской России, или описать как катастрофические изменения, которые даже сейчас не завершены и, возможно, влияют на здоровье и благополучие населения.
Еще до распада СССР рассматривался вопрос о необходимости серьезных изменений в системе здравоохранения страны. В действительности, рассматриваемые в данной статье проекты TACIS начались через 2–3 года после рождения нового государства.
Фактически, задолго до создания нового государства руководители СССР уже осознавали необходимость пересмотра и модернизации российских служб здравоохранения. В последние дни существования СССР лидеры в области здравоохранения признавали, что эта система больше не подходит для достижения всех поставленных целей. Ко второй половине 1980-х гг. министр здравоохранения СССР Е. Чазов поднимал вопрос о роли семейного врача. Эту позицию поддержал другой экс-министр здравоохранения И. Денисов, который рассматривал успешное внедрение семейной медицины и семейных врачей в Канаде в качестве возможного варианта в России [8, 9]. В некотором смысле уже были созданы предпосылки для таких инициатив, как проекты TACIS. Многие авторы обосновывали идеи Чазова и Денисова имеющимися в то время проблемами ПМСП и отмечали важность перехода к моделям семейной медицины [10–14].
К тому времени, когда первоначальные пилотные исследования TACIS по ОВП/СМ вышли из стадии разработки и получили статус активных экспериментальных исследований, в Российской Федерации был опубликован Федеральный закон «Основы законодательства Российской Федерации об охране здоровья» № 5487-1 от 22 июля 1993 г. (Российская Федерация, 1993–2007). В рамках этого документа статья 22 «Права семьи» включала следующую формулировку [15]:
«Государство берет на себя заботу об охране здоровья членов семьи.
Каждый гражданин имеет право по медицинским показаниям на бесплатные консультации по вопросам планирования семьи, наличия социально значимых заболеваний и заболеваний, представляющих опасность для окружающих, по медико-психологическим аспектам семейно-брачных отношений, а также на медико-генетические, другие консультации и обследования в учреждениях государственной или муниципальной системы здравоохранения с целью предупреждения возможных наследственных заболеваний у потомства.
Семья по договоренности всех ее совместно проживающих совершеннолетних членов имеет право на выбор врача общей практики (семейного врача), который обеспечивает ей медицинскую помощь по месту жительства.»
Таким образом, теперь семья на законных основаниях имела право на ориентированную на семью помощь и на выбор семейного врача. Примечательно, что в последнее время был издан обновленный закон — Федеральный закон Российской Федерации от 21.11.2011 № 323-ФЗ «Об основах охраны здоровья граждан в Российской Федерации» с изменениями от 29 декабря 2015 г. (Российская Федерация, 2011/2015). Соответствующая статья (теперь статья 51) перечисляет права членов семьи, которые во многом сходны, но в некоторых отношениях различны с представленными в предыдущей версии закона [16].
Предыстория текущего обзора
Этот обзор основан на анализе результатов многолетнего сотрудничества между представителями систем здравоохранения России и Северной Ирландии, начиная с конца 1980-х гг. Программа технического обмена, начатая в 1988 г., привела к участию Северной Ирландии в первой финансируемой Европейским Союзом программе реформирования системы здравоохранения в Советском Союзе. В 1993–1994 гг. был определен проект ЕС TACIS по поддержке развития систем здравоохранения, который осуществлялся с 1995 по 1998 г. Основной темой проекта стала поддержка развития ПМСП на базе ОВП в отдельных пилотных регионах России. В то время ПМСП оказывалась, как правило, терапевтами, акушерами-гинекологами и педиатрами, базирующимися в поликлиниках. Здесь не было ни врачей общей практики, ни семейных врачей.
Санкт-Петербург был одним из пилотных регионов, где должна была быть разработана и внедрена концепция ПМСП на основе ОВП/СМ. Три других региона, участвовавшие в проекте, — Самара (Приволжский регион), Екатеринбург (Уральский регион) и Кемерово (Западная Сибирь). Был разработан и согласован комплекс принципов, получивших название «Смольнинские принципы», которые должны были использоваться для реализации экспериментального проекта. Было создано 16 пилотных отделений ОВП (семейной медицины), по 4 в каждом пилотном регионе, и российские врачи ПМСП прошли обучение для оказания нового вида медицинской помощи. Первоначально обучение врачей общей практики проводилось в Белфасте (Северная Ирландия, Великобритания), но в дальнейшем стал использоваться подход подготовки инструкторов, что позволило обучать врачей в пилотных регионах России.
Правительство Российской Федерации и Комиссия Европейского Союза оценили проект TACIS как успешный. ПМСП, основанная на ОВП, была создана в короткие сроки, и услуги врачей общей практики стали доступными для небольшой, но значимой доли населения в каждом из пилотных регионов.
Если бы события тогда развивались в обычном русле, вряд ли было бы возможно дальнейшее взаимодействие российского и североирландского секторов здравоохранения в этой сфере деятельности. Однако, учитывая значимость и длительность установившегося сотрудничества, оно продолжалось и в последующие годы, особенно в Санкт-Петербурге. Параллельно с участием в дальнейших мероприятиях TACIS в Москве и Белгороде (проекты по развитию ПМСП, 2002–2005 гг.) и Калининграде (проект по улучшению показателей состояния здоровья населения Калининградской области, 2006–2010 гг.) поддерживался контакт с Комитетом по здравоохранению Правительства Санкт-Петербурга. Стало ясно, что из четырех пилотных регионов, участвующих в первом проекте TACIS, Санкт-Петербург демонстрирует наибольшие перспективы с точки зрения внедрения концепции ПМСП, основанной на ОВП.
В 2015 г. между Комитетом по здравоохранению Правительства Санкт-Петербурга и Ольстерским университетом было достигнуто соглашение о создании совместной исследовательской группы по вопросам политики в области здравоохранения, в компетенцию которой входил бы обмен информацией о системах здравоохранения и системах финансирования здравоохранения в Европейском Союзе и России, а также проведение совместных исследований по широкому кругу вопросов здравоохранения. Первая исследовательская программа, которая была предпринята группой, заключалась в том, чтобы сосредоточить внимание на характеристиках учреждений ПМСП в Санкт-Петербурге, в частности, насколько эти учреждения функционируют в соответствии со Смольнинскими принципами, разработанными в рамках первоначального проекта «Поддержка развития систем здравоохранения». Эта программа началась в 2015 г. и включала оценку текущей работы врачей общей практики (семейных врачей) в отдельных районах города. Полученные на сегодняшний день результаты представлены в следующих разделах, которым предшествует краткое описание используемых методов исследования.
Методологическая направленность
Методы, использовавшиеся для обзора деятельности с 2015 г. по настоящее время, были весьма разнообразными. Они основаны на оценочных методах, применявшихся при оценке первоначальных мероприятий пилотного проекта. В Приложении 1 описываются подходы, принятые в одном из таких пилотных проектов: «Улучшение состояния здоровья населения Калининградской области, 2006–2010 годы». По сути, методологическая направленность заключается в том, чтобы следовать принципам так называемого подхода быстрого обзора [17]. В каждом случае, опираясь на широкие цели пилотного проекта и проводя предварительное исследование [18], появлялась индивидуальная стратегия обзора. Это включало, как показано в Приложении 1, методы сбора и анализа данных, такие как анализ нормативных документов и планирования, фокус-группы пользователей и руководителей, углубленное собеседование, ознакомительные раунды Delphi, групповые интервью / обсуждения. Такой пример структуры был специфичен для калининградского проекта, но структура варьировала в зависимости от конкретных аспектов различных пилотных проектов.
В здравоохранении большое значение придается принципам научно-доказательной медицины и, по возможности, лечению и уходу, основанным на наилучших доступных количественных объективных научных данных (табл. 2) [19]. Однако признается, что здоровье и нездоровье и то, как они определяются, в высшей степени эмпирические вопросы. Таким образом, качественный субъективный аспект также имеет большое значение. С годами это признание только усилилось. С точки зрения доказательной медицины количественные и качественные исследования имеют ограничения, но при этом являются ценными источниками информации.
Таблица 2
Направления в исследованиях и практике [19]
Количественная ориентация | Качественная ориентация |
Объективные показатели | Субъективные показатели |
Поиск фактических данных | Поиск понимания |
Измерение явлений | Изучение смысла |
Упомянутое смешение методов в соответствии со спецификой ситуации, иногда называемое бриколажем, часто применяется в качественных социальных науках [20, 21]. Это опирается на французское слово bricoleur, которое относится к разнорабочему или мастеру на все руки. Характерной особенностью таких работников является их способность работать со множеством проблем в конкретных и часто уникальных обстоятельствах, используя не только стандартные инструменты, но и инструменты, которые они модифицировали или разработали для использования в определенных обстоятельствах. Это же делают исследователи-бриколеры. Они разрабатывают методы и даже модифицируют или разрабатывают конкретные инструменты в соответствии с конкретными проблемами или задачами исследования. Хотя для этого обзора не были разработаны совершенно новые инструменты исследования, дизайн запроса основывался на проблеме (развитие ПМСП) в конкретных уникальных ситуациях и не был строго привязан к жестким схемам обзора; таким образом, используя подходы быстрого обзора с реалистичной перспективой оценки [17–21]. Очевидно, что было необходимо закрепить обзор основных концепций ПМСП [22]. WONCA (The World Organization of Family Doctors) предложила шесть основных компетенций: управление первичной медицинской помощью, ориентация на сообщество, навыки решения конкретных проблем, комплексный подход, личностно-ориентированная помощь и целостная (холистическая) модель (рис. 3). Аналогичная структура, представленная Смольнинскими принципами, разработанными десятилетием ранее (Приложение 2), была явно прогрессивной в своей концептуализации и установила критерии для определения прогресса в развитии ОВП (семейной медицины).
Рис. 3. Принципы WONCA для общей врачебной практики (семейной медицины) [22]чебной практики (семейной медицины) [22]
Хотя в Санкт-Петербурге конкретная методология, изложенная в Приложении 1, не была использована, были применены основные методы: сбор информации, анализ, оценка и обзор нормативной базы, включая изучение документов, визиты наблюдателей, групповые обсуждения и интервью. Была осуществлена серия обзорных визитов, в ходе которых важнейшие аспекты рассматривались с участием ключевых заинтересованных групп. Таким образом, фактически была сохранена идея согласования метода обзора с изучаемым вопросом. Это было дополнительно структурировано с использованием Смольнинских принципов, разработанных и согласованных ранее в рамках инициативы TACIS (Приложение 2). На этой основе были рассмотрены вопросы, непосредственно вытекающие из указанных принципов (сбор информации, анализ данных / информации, выработка оценочных суждений и рассмотрение вопросов политики). Таким образом, были определены следующие девять проблем:
- позиционирование ОВП/СМ в системе здравоохранения;
- ОВП и семейная медицина;
- команда ПМСП;
- регистрация пациентов;
- комплексная (холистическая) помощь;
- профилактическая помощь;
- протоколы, стандарты и взаимодействие различных уровней медицинской помощи;
- мониторинг и оценка / обеспечение качества;
- образование и профессиональная подготовка / непрерывное профессиональное развитие.
Эти вопросы рассматриваются в нашей статье далее.
Позиционирование общей врачебной практики / семейной медицины в системе здравоохранения
За 20 лет, прошедших с момента завершения первоначального проекта TACIS, отмечено значительное развитие ОВП (семейной медицины) в Санкт-Петербурге. В настоящее время около 20 % населения города имеют доступ к ПМСП на базе ОВП, а в Приморском районе этот показатель достигает 40 %. Вопрос о доступности был поставлен на первое место после утверждения планов строительства новых жилых комплексов, включая требование о предоставлении соответствующих учреждений ПМСП. Один из принципов, на котором базируется развитие ОВП, заключается в том, что ПМСП на базе ОВП должна быть пунктом первого контакта населения со службой здравоохранения и являться предпочтительным местом для оказания всех медицинских услуг. Врач общей практики должен выступать в качестве привратника к необходимым услугам. Общая врачебная практика в настоящее время является первой точкой контакта со службой здравоохранения в тех районах, где она была создана, и врачи общей практики эффективно выполняют роль привратника. Эффективность этого подхода была продемонстрирована, например, в ходе мониторинга показателей направлений на госпитализацию. Было показано, что врачи общей практики, работающие в государственных медицинских организациях, направляют пациентов в стационары реже, чем традиционные поликлинические бригады ПМСП. Отдельные статистические данные о количестве обращений по общим практикам, действующим в рамках инициативы государственно-частного партнерства, отсутствуют.
Такое сокращение числа направлений пациентов на госпитализацию врачами общей практики может привести к повышению экономической эффективности системы здравоохранения в целом за счет ограничения объема более дорогостоящей стационарной помощи. Учитывая, что 80 % пациентов в городе по-прежнему получают первичную медицинскую помощь в поликлиниках, а также связанные с этим более высокие показатели направления на стационарное лечение, существует определенный путь для достижения оптимальной экономической эффективности. Это косвенно признается Комитетом по здравоохранению, уделяющим значительное внимание развитию ОВП, что отмечено в стратегическом плане до 2024 г. Вместе с тем следует отметить, что не было установлено никаких конкретных целевых показателей для расширения охвата ОВП. Представляется вероятным, что в отсутствие таких целевых показателей сроки достижения всеобщего охвата будут значительно увеличены. Еще одним предварительным условием для усиления экономического эффекта от ОВП является перевод финансовых ресурсов из стационаров в учреждения ПМСП в соответствии с сокращением числа направляемых на госпитализацию пациентов. В настоящее время нет никаких свидетельств того, что такие финансовые операции осуществляются или планируются.
В соответствии с упомянутой концепцией «привратника», доступ к специализированным услугам должен осуществляться только по направлению врача общей практики за исключением несчастных случаев и чрезвычайных ситуаций. Очевидно, что в ситуации, когда 80 % населения не имеют доступа к услугам врачей общей практики, в общегородском масштабе это пока невыполнимо. Однако обнадеживает тот факт, что там, где существуют услуги врачей общей практики, пациенты охотно соглашаются на такую организацию медицинской помощи. Это говорит о том, что при достижении всеобщего охвата ОВП концепция «привратника» станет реальностью, независимо от того, будет ли отменено законодательное положение, позволяющее пациентам консультироваться с врачом по своему выбору.
Общая врачебная практика и семейная медицина
В Европе ОВП и семейная медицина обычно рассматриваются как одна специальность. В России эти термины, как правило, трактуются по-разному: считается, что врачи общей практики оказывают медицинские услуги только взрослым, в то время как семейные врачи оказывают медицинские услуги всей семье, включая детей. В соответствии с Федеральным законодательством медицинские услуги должны быть предоставлены детскому населению отдельно от взрослого. В ходе нашего визита в медицинские учреждения в феврале 2019 г. мы отметили, что данная проблема была решена лишь в некоторых отделениях общей врачебной практики, включая и те, которые участвуют в реализации инициативы государственно-частного партнерства (ГЧП). При условии заключения договора со взрослыми и детскими поликлиниками медицинские организации ГЧП могут предоставлять услуги общей врачебной практики всей семье, в том числе общетерапевтические, акушерские/гинекологические и педиатрические.
Некоторые государственные медицинские учреждения функционируют на основе принципов семейной медицины. В частности, 2 клиники семейной медицины в Калининском районе Санкт-Петербурга, 3 — в Приморском и 1 — в Выборгском предоставляют медицинское услуги и взрослым и детям. Некоторые из посещенных нами медицинских организаций являются государственными. Это говорит о том, что те государственные учреждения, которые считают, что действующее законодательство мешает им развивать истинную семейную медицину, могут в конечном итоге найти способ изменить эту ситуацию.
Потребность в отдельных услугах для взрослых и детей имеет меньшее значение на уровне поликлиники. Если у отделения ОВП и, в идеале, у конкретного врача общей практики, есть представления о состоянии здоровья всей семьи, не менее важно, чтобы вспомогательные услуги, предоставляемые другими медицинскими организациями, также предоставлялись в одной организации.
Мы были впечатлены моделью здравоохранения, которая в настоящее время появляется в Санкт-Петербурге и включает в себя не только ОВП/СМ и стационарное лечение, но и промежуточную помощь, предоставляемую реконструированными поликлиниками. Поликлиники по-прежнему предоставляют традиционные услуги ПМСП для 80 % городского населения, но часть из них предоставляет дополнительную консультативную помощь для пациентов врачей общей практики, что расширяет вклад ПМСП в общее оказание медицинской помощи. На более ранней стадии процесса реформирования существовала точка зрения, что ОВП должна постепенно заменять поликлинические услуги, и что поликлиники в конечном итоге прекратят свое существование.
Опыт Великобритании в целом и Северной Ирландии в частности показывает, что существуют ограничения для бинарной модели оказания медицинской помощи. В настоящее время ОВП в Северной Ирландии чрезмерно перегружена настолько, что, за исключением случаев крайней необходимости, пациентам приходится ждать 3–4 недели, чтобы записаться на прием к своему врачу общей практики. В то же время амбулаторные отделения стационаров переполнены пациентами, которые могли бы пользоваться услугами врача общей практики. Развитие промежуточного уровня медицинской помощи в Северной Ирландии, на уровне ПМСП, но более специализированного, чем ОВП, может одновременно поддержать и врачей общей практики, и оказание амбулаторной помощи в стационарах. Было бы нецелесообразно начинать строительство новых поликлиник, поэтому наилучшим вариантом может стать организация клиник, в которых амбулаторно будут принимать врачи стационаров.
Санкт-Петербург находится в удачном положении благодаря существующей инфраструктуре поликлиник, которые могут постепенно трансформироваться из предоставления услуг ПМСП первого уровня по традиционной модели в оказании помощи среднего уровня в поддержку развивающейся сети ОВП. В настоящее время поликлиники предлагают оба вида услуг на переходном этапе развития ПМСП и, похоже, делают это очень успешно.
Команда первичной медико-санитарной помощи
Принцип, согласно которому услуги ОВП должны предоставляться командой ПМСП, состоящей из врачей общей практики, медицинских сестер, социальных работников и других специалистов первичного звена, в настоящее время достаточно хорошо соблюдается в Санкт-Петербурге. Традиционные установки, определяющие медсестру как помощника врача, уходят в прошлое. Медицинские сестры в бригадах ПМСП теперь имеют свои собственные роли, наиболее значимые в области профилактики, скрининговых услуг и иммунизации. Что касается профилактики, медсестры принимают активное участие в ведении регистров, организации приема лекарств, проведении визитов на дом, предоставлении информации о сдаче анализов крови и т. д.
Существуют некоторые свидетельства более активного вовлечения социальных работников в работу команды ПМСП, но пока это взаимодействие развито недостаточно. Социальные работники находятся под отдельным административным контролем, что усложняет процесс их привлечения в бригады первичной медицинской помощи.
Представители Фонда обязательного медицинского страхования часто находятся в поликлиниках, и с ними могут консультироваться пациенты, в том числе зарегистрированные у врачей общей практики.
Многие специалисты ПМСП, например физиотерапевты, не часто входят в состав команд ОВП, но их услуги обычно доступны для пациентов в других поликлиниках. Это справедливо как для государственной общей практики, так и для практики ГЧП, хотя, как представляется, эти связи легче устанавливаются государственными ведомствами. Некоторые практики ГЧП уделяют большое внимание интеграции с государственной системой, но сталкиваются с некоторыми препятствиями в достижении этой цели. Особенно часто возникают вопросы в области иммунизации детей и скрининга.
Регистрация пациентов
Принцип ОВП заключается в том, что каждый пациент должен быть зарегистрирован, чтобы обеспечить непрерывность и преемственность ухода, принимая во внимание всю прошлую медицинскую, психологическую и социальную историю пациента и его/ее семьи. Сейчас это повсеместно имеет место в тех районах Санкт-Петербурга, где развита ОВП. В государственной медицинской организации пациентов регистрируют, используя, например, автоматическую систему регистрации. Практики ГЧП имеют свои собственные механизмы регистрации.
Регистрация в поликлиниках не гарантирует непрерывности или преемственности медицинской помощи, поскольку пациенты, вероятно, будут осматриваться разными врачами в разных случаях. Регистрация в базе данных в ОВП делает непрерывность оказания медицинской помощи более вероятной ввиду меньшего размера команды и более ориентированного на пациента подхода.
Холистический (целостный) подход
Еще один принцип ОВП заключается в том, что при ведении пациента команда ПМСП должна применять целостный подход с учетом всех психосоциальных обстоятельств. Мы увидели применение такого подхода при оказании медицинской помощи в отделениях ОВП, которые посетили в Санкт-Петербурге.
Профилактическая помощь
В соответствии с еще одним принципом ПМСП на базе ОВП, существуют услуги, которые выходят за рамки лечебной деятельности, включающей скрининг, лечение хронических заболеваний, укрепление здоровья и профилактику заболеваний. Существует специальная линия финансирования из фонда обязательного медицинского страхования для покрытия этих услуг, и выплаты основаны на ряде показателей, разработанных для этой цели. Эти услуги включают диспансеризацию и профилактические осмотры, охват которыми в настоящее время составляет 48 %, а к 2024 г. должен достичь 96 % пациентов. Предполагается, что работодатели будут предоставлять сотрудникам 1–2 дня в год для профилактических посещений медицинских учреждений, что подтверждает понимание государством преимуществ профилактики. В области лечения хронических заболеваний были созданы специальные центры для лечения диабета и хронических сердечно-сосудистых заболеваний. Как упоминалось ранее, медицинские сестры принимают активное участие в этой работе.
Медицинская документация пациентов, содержащая полную информацию о них, — важная предпосылка для целостного подхода, включая скрининг, выявление групп риска и ведение хронических заболеваний. Отметим, что процессы ведения документации эффективно организованы на всех уровнях системы в Санкт-Петербурге, и во многом благодаря этому, а также приоритету, придаваемому профилактике, достигнут столь значительный прогресс по всем аспектам профилактической помощи.
Протоколы, стандарты и взаимодействие различных уровней медицинской помощи
Авторам пока не удалось подробно изучить область протоколов и стандартов, используемых для регулирования деятельности в рамках ПМСП. Однако нам известно об инициативах, которые были предприняты для регулирования деятельности на стыке первичной и специализированной медицинской помощи и, по сути, между различными уровнями системы первичной медицинской помощи. В Приморском районе был реализован интересный проект по изучению потоков пациентов внутри и вне поликлиники. Информация, полученная в ходе этого проекта, позволяет врачам более эффективно направлять пациентов к специалистам поликлиники (в том числе в качестве поддержки ОВП), на лабораторные и инструментальные исследования, а также на высокотехнологичные исследования или на госпитализацию.
Мониторинг и оценка / обеспечение качества
Мониторинг и оценка объема, доступности и качества услуг является одним из важнейших компонентов системы ПМСП. Постоянная оценка потребностей и приоритетов в области здравоохранения, а также эффективность ответных мер в этой области имеют решающее значение для повышения качества, эффективного использования ресурсов и развития сферы услуг. Мы слышали об интересном пилотном проекте в поликлинике № 57 Невского района, предполагающем внедрение японских подходов к управлению («бережливая поликлиника». — прим. редактора). Хотя эта работа еще находится на экспериментальной стадии, она демонстрирует значительные перспективы более эффективного с точки зрения затрат подхода к предоставлению услуг и потенциально может внести значительный вклад в текущую оценку удовлетворения потребностей пациентов.
Опыт многих европейских стран свидетельствует, что особое внимание следует уделять созданию механизма, позволяющего включать результаты исследований качества услуг в процесс стратегического планирования. Этот непрерывный цикл разработки политики, стратегического реагирования, предоставления услуг, оценки и мониторинга, ведущий к дальнейшему развитию соответствующей политики, требует структурированного участия представителей комитетов здравоохранения, страховых медицинских организаций, академических структур и медицинских организаций через профессиональные ассоциации. Такой механизм будет способствовать тому, чтобы уроки, извлеченные из оценки, в том числе из экспериментальных проектов, были учтены и применены для развития системы здравоохранения.
На сегодняшний день мы не обладаем исчерпывающей информацией для полной оценки механизмов обеспечения качества и их включения в процесс планирования.
Образование и профессиональная подготовка / непрерывное профессиональное развитие
В 2011 г. Санкт-Петербургская государственная медицинская академия и медицинская академия последипломного образования объединились в Северо-Западный государственный медицинский университет им. И.И. Мечникова. Новый университет обеспечивает обучение по поликлинической терапии для студентов последнего курса и обучение по ОВП в ординатуре и на циклах профессиональной переподготовки. Врачи общей практики также обучаются в других медицинских университетах Санкт-Петербурга [1].
Университет по-прежнему обеспечивает подготовку участковых врачей-терапевтов, но включает в учебный план коммуникативные навыки, вопросы комплексного подхода, непрерывности медицинской помощи, ухода за пожилыми людьми и паллиативной помощи, тем самым приводя обучение в большее соответствие с ОВП. С 2017 г. все студенты-выпускники должны проходить процедуру аккредитации, после чего они могут занять должность врача-терапевта участкового (без обучения в ординатуре и пройдя всего 6,5 недель обучения по поликлинической терапии на последнем курсе). Этот режим обучения участковых терапевтов явно недостаточен для обеспечения того, чтобы традиционные поликлинические бригады могли оказывать целостную первичную помощь, сопоставимую с той, которую оказывают врачи общей практики / семейные врачи, и еще раз подчеркивает важность перехода к универсальному охвату населения ОВП/СМ в Санкт-Петербурга.
Заключение
В целом, прогресс, достигнутый в развитии ОВП/СМ за последние 20 лет, впечатляет. Не все возможно изменить, но как указывалось ранее, есть аспекты развивающихся услуг, которые можно было бы с пользой рассматривать в качестве вклада в продолжающуюся дискуссию о реформе системы здравоохранения в Северной Ирландии. Мы предлагаем следующие аспекты для рассмотрения Комитетом по здравоохранению, чтобы ускорить реализацию стратегического плана до 2024 г. в отношении развития ОВП как основной модели оказания ПМСП.
- При реализации стратегического плана было бы полезно ввести поэтапные целевые показатели для развития ОВП/СМ, например целевой показатель охвата определенной процентной доли городского населения к определенным датам; таким образом, сроки достижения всеобщего охвата могут быть значительно сокращены.
- По мере расширения ОВП/СМ поликлиники должны продолжать развиваться как поставщики услуг промежуточного уровня между ОВП/СМ и стационарами.
- Чтобы в полной мере реализовать экономические выгоды перехода к ОВП/СМ, необходимо создать механизмы, обеспечивающие постепенный перевод ресурсов со стационарной помощи на первичную по мере увеличения охвата ОВП/СМ и снижения числа госпитализаций.
- Опираясь на опыт тех практик, которые уже достигли этого, следует удвоить усилия по поиску путей преодоления препятствий на пути развития истинной семейной медицины, устранив тем самым различие между ОВП (для взрослых) и семейной медициной (для взрослых и детей).
- Хотя существующие подходы к мониторингу и оценке качества не были проанализированы, предлагается двухэтапная текущая / формирующая и суммирующая оценка, включающая клинический аудит и основанная на протоколах, составленных из фактических данных, в соответствии со статьей 10 Смольнинских принципов (см. Приложение 2).
- Следует предпринять усилия по дальнейшей адаптации программ подготовки участковых терапевтов для облегчения оказания более целостной первичной медицинской помощи в ожидании реализации всеобщего охвата ОВП/СМ для Санкт-Петербурга.
В дальнейшем было бы интересно аналогичным образом рассмотреть прогресс в развитии ОВП/СМ в других регионах Российской Федерации, где были завершены пилотные проекты по реформированию ПМСП.
Приложение 1
Образец быстрого обзора
Приложение 2
Смольнинские принципы
Комплекс принципов, определяющих развитие первичной медико-санитарной помощи на основе общей врачебной практики (семейной медицины) в Российской Федерации, принятый на конференции в рамках проекта Европейского Союза TACIS «Поддержка развития системы здравоохранения» (октябрь 1995 г., Санкт-Петербург, гостиница «Смольнинская»).
- Первичная медико-санитарная помощь на основе модели общей врачебной практики (семейной медицины) должна быть пунктом первого контакта населения со службой здравоохранения и предпочтительным местом для оказания всех медицинских услуг.
- Медицинская помощь первого контакта должна быть доступна для всех членов семьи, независимо от повода к обращению.
- Врач общей практики (семейный врач) должен выполнять роль привратника при оказании медицинской помощи. Консультации врачей-специалистов и госпитализации должны осуществляться по направлению врача общей практики (за исключением несчастных случаев и неотложных ситуаций).
- Медицинская помощь должна оказываться командой первой медико-санитарной помощи, состоящей из врачей общей практики, медицинских сестер, социальных работников и других специалистов первичного звена, с учетом конкретных потребностей обслуживаемого населения (гендерные и возрастные особенности, заболеваемость и т. д.).
- Каждый пациент должен быть зарегистрирован в базе данных отделения общей врачебной практики, чтобы обеспечить непрерывность и преемственность оказания медицинской помощи с учетом медицинского, психологического и социального анамнеза пациента и его семьи.
- При оказании медицинской помощи в общей врачебной практике необходимо обеспечить холистический (комплексный) подход, учитывающий психосоциальные особенности пациента.
- Предоставляемые услуги должны выходить за рамки лечебной помощи и включать скрининг, лечение хронических заболеваний, укрепление здоровья и профилактику заболеваний.
- В общей врачебной практике должен вестись полный учет пациентов, чтобы обеспечить целостный подход к медицинской помощи, включая скрининг, выявление групп риска и лечение хронических заболеваний.
- Следует разработать протоколы и стандарты для регулирования деятельности в рамках команды первичной медико-санитарной помощи (общей врачебной практики) и при взаимодействии первичной и специализированной медицинской помощи.
- Для оценки эффективности работы членов команды должны внедряться процедуры обеспечения качества, основанные на проведении клинического аудита, помимо показателей, основанных на данных научно-доказательной медицины.
- Работа команды должна сопровождаться непрерывным профессиональным развитием и мотивироваться стимулами, направленными на поощрение соблюдения указанных ранее принципов.
Примечания:
* Группа по исследованиям и разработкам в области здравоохранения была создана в 2006 г. как подразделение, занимающееся вопросами международного развития на факультете здравоохранения и наук о жизни Университета Ольстера.
* The Healthcare Research & Development Group was established in 2006 as an international development unit within the Health & Life Sciences faculty of the University of Ulster.
Об авторах
Уел Гиллан
Группа исследования и развития здравоохранения*, Ольстерский университет
Автор, ответственный за переписку.
Email: gillan47@hotmail.com
бакалавр медицинских наук, бакалавр хирургии, бакалавр акушерства и гинекологии, специалист первичного звена здравоохранения
Ирландия, Белфаст, Северная ИрландияРоб Маккуистон
Группа исследования и развития здравоохранения*, Ольстерский университет
Email: rob_mcquiston@hotmail.com
бакалавр экономических наук, доктор философии, специалист по организации и управлению в здравоохранении
Ирландия, Белфаст, Северная ИрландияОливер Слевин
Группа исследования и развития здравоохранения*, Ольстерский университет
Email: oliver.slevin@gmail.com
бакалавр гуманитарных наук, магистр гуманитарных наук, специалист общего сестринского дела, специалист сестринского дела в области психических заболеваний, специалист-преподаватель, специалист по образованию и управлению
Ирландия, Белфаст, Северная ИрландияСписок литературы
- Shkolnikov V, Meslé F. The Russian epidemiological crisis as mirrored by mortality trends. In: J. Da Vanzo, G. Farnsworth, ed. Russia’s demographic crisis. RAND: Santa Monica, CA; 1996.
- United Nations. Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. World Population Prospects; 2019 [accessed 2019 Dec 12]. Available from: https://population.un.org/WPP/Download/.
- World Bank. Population estimates and projections. Washington DC: The World Bank; 2019 [accessed 2019 Dec 12]. Available from: https://datacatalog.worldbank.org/dataset/population-estimates-and-projections.
- Bobylev Yu, Bozhechkova А, Mkrtchan N, et al. Monitoring of Russia’s economic outlook: trends and challenges of socio-economic development, No. 12. Russian Presidential Academy of National Economy and Public Administration; 2019. 16 p.
- Ferris-Rotman A. Putin’s next target is Russia’s abortion culture. Foreign Policy; 2017.
- Rozenfeld BA. The crisis of Russian health care and attempts at reform. In: Russia’s demographic crisis. Ed. by J. Da Vanzo, G. Farnsworth. RAND: Santa Monica, CA; 1996.
- Toon PD, Vilks T, Schlachter K, et al. Reforming the Russian health service. Otherwise it might be convenient. Urgent aid, chronic penalties. Professional law breakers. Training general practitioners in Saint Petersburg. Training general practitioners in Gatchina. BMJ. 1998;317(7160):741-744. https://doi.org/10.1136/bmj.317.7160.741.
- Ryan M, Stephen J. General practitioners and family doctors in the Russian Federation. Br J Gen Pract. 1996;46(409):487-489.
- Sakhanovskaya M. Semeiny vrach v interere vuza. Meditsinskaya gazeta. 1993;22:8-9.
- Rese A, Balabanova D, Danishevski K, Implementing general practice in Russia: getting beyond the first steps. BMJ. 2005;331(7510):204-207. https://doi.org/10.1136/bmj.331.7510.204.
- Russia’s demographic crisis. Ed. by J. Da Vanzo, G. Farnsworth. RAND: Santa Monica, CA; 1996.
- Vertakova J, Vlasova O. Problems and trends of Russian health care development: 21st International Economic Conference 2014, IECS 2014, 16–17 May 2014, Sibiu, Romania. Procedia Economics and Finance. 2014;16:34-39. https://doi.org/10.1016/S2212-5671(14)00771-0.
- Groenewegen PP, Dourgnon P, Greß S, et al. Strengthening weak primary care systems: Steps towards stronger primary care in selected Western and Eastern European countries. Health Policy. 2013;113(1-2):170-179. https://doi.org/10.1016/j.healthpol.2013.05.024.
- Starfield B. Toward international primary care reform. CMAJ. 2009;180(11):1091-1092. https://doi.org/10.1503/cmaj.090542.
- Fundamentals of the legislation of the Russian Federation on health protection no. 5487-1 of July 22, 1993 (with the additions and amendments of December 24, 1993, March 2, 1998, December 20, 1999, December 2, 2000, January 10, February 27, June 30, 2003, June 29, August 22, December 1, 29, 2004, March 7, December 21, 31, 2005, February 2, December 29, 2006, July 24, October 18, 2007). Available from: https://www.wto.org/english/thewto_e/acc_e/rus_e/WTACCRUS58_LEG_270.pdf.
- Russian Federation. Federal Law of the Russian Federation No. 323-FZ of 21.11.2011 on Basics of health protection of the citizens in the Russian Federation as amended to 29 December 2015. International Labour Organization; 1996–2014. Available from: https://www.ilo.org/dyn/natlex/natlex4.detail?p_lang=en&p_isn=102297.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19-32. https://doi.org/10.1080/1364557032000119616.
- Khangura S, Konnyu K, Cushman R, et al. Evidence summaries: the evolution of a rapid review approach. Syst Rev. 2012;1:10. https://doi.org/10.1186/2046-4053-1-10.
- Slevin O. Approaches to healthcare research. In: Healthcare research: a textbook for students and practitioners. Ed. by P. Roberts, H. Priest. Chichester, UK: John Wiley & Sons Ltd; 2010.
- Kincheloe JL. Describing the bricolage: conceptualizing a new rigor in qualitative research. Qualitat Inq. 2001;7(6):679-672. https://doi.org/10.1177/107780040100700601.
- Kincheloe JL. Redefining and interpreting the object of study. In: Rigour and complexity in educational research: conceptualizing the bricolage. Ed. by J.L. Kincheloe, K.S. Berry. Maidenhead: Open University Press; 2004.
- World Organisation for National Colleges and Academies of General Practice / Family Medicine. The European definition of general practice / family medicine: 2011 Edition. WONCA Europe; 2011. Available from: https://www.woncaeurope.org/sites/default/files/documents/Definition%203rd%20ed%202011%20with% 20revised%20wonca%20tree.pdf.
Дополнительные файлы