The importance of immunohistochemical examinations for patients with failed IVF-methods
- Authors: Abramova V.N.1, Gajdukov S.N.1, Tajc A.N.1
-
Affiliations:
- St Petersburg State Pediatric Medical University
- Issue: Vol 8, No 1 (2017)
- Pages: 82-88
- Section: Articles
- URL: https://journals.eco-vector.com/pediatr/article/view/6120
- DOI: https://doi.org/10.17816/PED8182-88
- ID: 6120
Cite item
Abstract
Infertility is one of the most acute problems in modern reproductive studies. The theme of research is poorly conceptualized in modern medical literature, and this fact is an additional confirmation of the relevance and scientific significance of this research. With the use of assisted reproductive technology (ART), pregnancy in an infertile marriage became possible. In this article, the authors pay significant attention to the role of the endometrium in the implantation process. To better assess the status of the endometrium, they performed hysteroscopy and endometrial biopsy and conducted morphological study of biopsy material and immunohistochemistry analysis. The features, competitive advantages, or disadvantages of every method of research and treatment have also been included in the discussion. Analysis of the results of the immunohistochemical studies revealed the presence of autoimmune chronic endometritis and chronic endometritis without an autoimmune component. Comprehensive examination and treatment resulted in successful pregnancy in 90% of women with failed IVF attempts in anamnesis. At the same time, in 60% of cases the pregnancy resulted in childbirth between 36 and 40 weeks of gestation. During such pregnancies, there are only a few specific features: high risk of miscarriage, fetal defects, and extragenital pathology. Thus, reproductology is in constant search for new methods that are able to further improve the positive results of IVF.
Full Text
Infertility is a serious reproductive problem that includes a combination of social and mental illnesses in the family (WHO, 1979). Infertility issues continue to be relevant and of high priority in obstetrics and gynecology because of its consistently high prevalence worldwide [1, 2]. Currently, there are more than six million married couples of reproductive age in Russia, of which three million need treatment using assisted reproductive technologies (ART) [6]. The number of infertile women is increasing. Thus, in 2007, there were 485.1 infertile women per 100,000 women of reproductive age, and in 2011, this figure increased to 559.6 [7].
A successful implantation requires a receptive endometrium and a normal interaction between the endometrium and embryo [12]. The role of the endometrium during implantation is often underestimated. Currently, chronic inflammatory processes involve not only the functional but also the non-incompatible basal layer of the endometrium [4]. Chronic endometritis is caused by immunodeficiency because of previous sexually transmitted infections, due to their long persistence, and presence of chronic somatic pathology [8]. The role and functional activity of the immune system, especially local immunity factors such as pro-inflammatory and regulatory cytokines, growth factors, adhesion molecules, matrix metalloproteinases, and apoptosis regulators, are of utmost importance in this pathology. In this case, immunological changes in the endometrium are in some cases an independent cause of infertility and miscarriage.
Chronic endometritis is accompanied by multiple morphofunctional changes such as cell proliferative disorder, apoptosis, angiogenesis, and fibrosis. In this case, a sharp activation of cellular and humoral factors of inflammation occurs at the local level. Notably, in the pathogenesis of chronic endometritis, there is a malfunction of immune regulatory mechanisms, which is manifested by the autoimmune nature of the immune response and increased endometrial content of CD16, natural killer, and B-cells [10]. Long-term stimulation of immunocompetent endometrial cells with an infectious agent leads to the decompensation of local homoeostatic regulatory mechanisms, which supports the persistence of the infectious process.
The “uterine factor” of infertility is found in more than half of women of reproductive age. The prevalence of chronic endometritis is the highest in women aged 26-35 years, accounting for 96.7%, which is very important in the implementation of reproductive function [10].
The aim of the study was to evaluate the efficiency of additional diagnostic methods, including pelvic ultrasound examination, hysteroscopy, endometrial biopsy, morphological examination of biopsy material, and immunohistochemistry (IHC) in infertile women and those who had unsuccessful ART programs.
MATERIALS AND METHODS
In 2014-2015, according to the records of the gynecological department of the Perinatal Center of Saint Petersburg State Pediatric Medical University, 50 women aged 26-43 years with infertility or unsuccessful in vitro fertilisation (IVF) attempts in the past were examined and treated. The study involved 20 patients admitted to the hospital to prepare them for a second IVF attempt after an unsuccessful ART.
Ten patients had a history of bacterial and viral diseases of the pelvic organs and underwent intrauterine interventions. Patients received antibiotics and antiviral drug therapy, and ART was performed after confirmation of negative bacterial and viral infections via PCR, but pregnancy did not occur.
IVF was planned for all women in the near future; therefore, verifying the uterine factor of infertility has become urgent. Patients studied were divided into two groups. Group 1 included women with endometrial pathology according to the ultrasound examination of the small pelvis and with unsuccessful ART, whereas group 2 included women without visible pathology on ultrasound examination of the small pelvis but with unsuccessful VRT. Patients underwent ultrasound examination followed by hysteroscopy, endometrial biopsy, histoanalysis of the uterine cavity scraping, and IHC. Hysteroscopy combined with endometrial biopsy, morphological examination of the endometrium, and IHC were performed on day 23 of the menstrual cycle. This combination aided in establishing accurate diagnosis and treatment of endometrial pathology.
Ultrasound examination of the pelvic organs was performed using high-technology equipment such as the expert-class Philips device equipped with sensors for all types of 3D or 4D studies. This device has the functions of Doppler ultrasound examination and elastography. A hysteroscopic resectoscope (Richard Wolf Medical Instruments, IL, USA) was used for hysteroscopy. IHC reactions were performed in paraffin sections using the peroxidase-antiperoxidase method with epitope retrieval in a microwave oven. Mouse monoclonal antibodies to estrogen receptors (ERs) and progesterone receptors (PRs) were used.
Using the IHC method, local immunity parameters, such as the number of lymphocytes expressing markers of natural killer cells CD56+ and CD16+ and activation markers HLA-DR (II)+, in the endometrial tissue were determined [5]. These parameters (i. e., CD56+, CD16+, and HLA-DR (II)+) were quantified by observing the endometrial scraping using an optical microscope with 400× magnification in three fields of vision [9].
RESULTS OF THE STUDY
The examinations revealed that eight patients suffered from primary infertility and 12 patients from secondary infertility. The number of IVF attempts in the group of examined women was 1-4. All patients had gynecological disorders in the family history (Table 1).
Table 1. Gynecological diseases of the examined women
Таблица 1. Структура гинекологических заболеваний обследованных женщин
Gynecological pathology | Number of cases | |
Uterus impaired development (bicornuate, arcuate, and incomplete intrauterine septum) | 1 | |
Oothecoma | 2 | |
Endometrial disease | 2 | |
Uterine myoma | 1 | |
Chronic salpingitis, oothecitis | 10 | |
Carrier state of human papilloma virus, uterine cervix pathology | 3 | |
Chlamydiosis, ureaplasmosis, mycoplasmosis, and cytomegalovirus infection | 12 | |
Endometrial polyp | 3 | |
Immunohistochemical data | Number of cases | |
Expression of estrogen and progesterone receptors in the endometrium does not correspond to menstrual cycle phases | 8 | |
Expression of estrogen and progesterone receptors in the endometrium corresponds to menstrual cycle phases | 12 | |
Autoimmune chronic endometritis: | 11 | |
Primary | 2 | |
Inactive | 9 | |
Chronic endometritis without an autoimmune component: | 8 | |
With exacerbation | 3 | |
Without exacerbation | 5 | |
Absence of endometritis | 1 | |
Among the concomitant diseases were diabetes mellitus type 2, obesity, autoimmune thyroiditis, and fibroadenoma of the mammary glands.
Patients were divided into groups according to the presence or absence of endometrial pathology based on the results of the ultrasound examination. Of the 20 women, 13 (65%) had polyps and endometrial hyperplasia. In the ultrasound examination, endometrial and myometrial changes, which are characteristics of inflammatory processes, were determined. Thus, small hyperechogenic inclusions were found in the projections of the basal layer, which persisted regardless of the menstrual cycle phase; diffuse, focal, and cystic changes, as well as varicose myometrium veins, were noted in the subendometrial zone; coarse closing line of the mucosa layers is observed. Color Doppler ultrasound revealed a relatively scarce vascularization of the functional layer in the secretory phase of the menstrual cycle, violation of hemodynamics in uterine vessels and vascular pool of thesmall pelvis, asymmetric myometrium vascularization (in 49% of cases), decreased final diastolic velocity in uterine arteries, and increased angular-dependent indices of the blood flow-velocity curves at all levels of the uterine vascular tree, which coincides with literature data [13].
All patients from the study group underwent additional diagnostic methods, such as diagnostic hysteroscopy, endometrial biopsy, morphological examination of the uterine cavity scraping, and IHC study.
In hysteroscopy, uneven thickness of the endometrium, polypoid vegetations, petechial hemorrhages, focal hypertrophy of the mucosa, and synechia in the uterine cavity were observed. Note that with suspected chronic endometritis, hysteroscopy of the entire intrauterine pathology is very important. Then, an endometrial biopsy with morphological examination should be performed in all cases to verify the diagnosis.
Morphological study was used to detect the presence of focal or diffuse periglandular and perivascular lymphohistiocytic inflammatory infiltrates in the basal and functional endometrial layers, plasma cells in the infiltrates, focal fibrosis of the stroma, and sclerotic changes in the walls of the spiral arteries of the endometrium, which coincides with literature data [3].
As previously mentioned, 15 patients (75%) had endometrial pathology in the form of polyps and endometrial hyperplasia, among which eight had glandular and fibroglandular polyps and seven had glandular endometrial hyperplasia. From the data presented, ultrasound examination for diagnosis is not highly informative, although it is a good method of revealing pathologies. Moreover, employing additional diagnostic methods aids in the diagnosis of chronic endometritis.
The final stage of the study was IHC. Diagnostic methods were proposed because inflammation often develops only locally, which affects organ function, and is always accompanied by changes in systemic and local immune parameters.
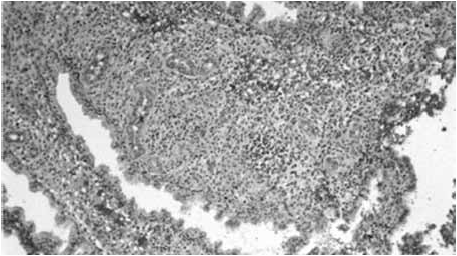
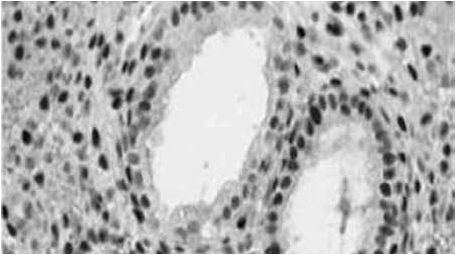
Analysis of IHC results revealed the presence of chronic endometritis with and without an autoimmune component. In terms of the receptor status of the endometrium in infertile women, chronic endometritis was accompanied by a decrease in ER expression in the glands in both the proliferative and secretory phases, but was mainly in the secretory phase in the stroma (Figure 1). PR expression in the glands and endometrial stroma decreases in the secretory phase (Figure 2).
Fig. 1. Estrogen receptors
Fig. 2. Progesterone receptors
The results of the IHC analysis are presented in Table 2.
Table 2. Results of immunohistochemical study
We analyzed the IHC results of a 29-year-old patient, who was admitted with primary infertility. The patient had morphologically confirmed fibroglandular polyps of the endometrium, which was previously identified by ultrasound examination.
Based on the findings of IHC analysis, ER and PR expression in the endometrium correspond to menstrual cycle phases (Figure 3). In addition, signs of chronic inflammation (i. e., chronic endometritis) with a weak autoimmune component (Figures 4-10) are revealed.
Fig. 3. Endometrial scraping during the late secretory phase at 100× magnification
Fig. 4. Focal lymphocytic and neutrophil infiltration of the endometrial stroma at 400× magnification
Fig. 5. Vacuolar dystrophy of gland epithelium and endometrial stroma at 1,000× magnification
Fig. 6. Expression of CD16 receptors
Fig. 7. Expression of CD56 receptors
Fig. 8. HLA-DR (II) receptors
Fig. 9. Estrogen receptors
Fig. 10. Progesterone receptors
After the final diagnosis of chronic endometritis, 19 women were treated according to the examination results. Patients with endometrial hyperplasia were treated with gestagens (Lindinet-30, Jeanine, Yarina) for three menstrual cycles followed by ultrasound monitoring. Women with endometrial polyps had no special hormonal treatment.
Treatment consisted of two stages. At the first stage, antimicrobial therapy entailed the combinations fluoroquinolones and nitroimidazoles, macrolides and nitroimidazoles, and antiviral therapy with tablet and vaginal preparations of Valtrex and Viferon. To increase the efficacy of anti-infective therapy, immunomodulators, such as Galavit and ImmunoMax, were used. Longidaza was also prescribed. At the second stage, patients underwent metabolic and systemic enzyme therapy with Actovegin and Wobenzym.
After comprehensive examination and treatment, 18 patients (90%) had an onset of pregnancy. It is noteworthy that in 12 cases, the pregnancy ended with childbirth within 36-40 weeks, of which there were twins in two cases. All children were born in satisfactory conditions and an Apgar score of >7 points. In four cases, premature delivery occurred at 23-29 weeks of gestation (22.2%). In one case, postnatal fetal death occurred. Retention of dead ovum was noted in two cases (11.1%) within 7-8 weeks of pregnancy, which required scraping of the uterine cavity.
CONCLUSION
In conclusion, analysis of the obtained results revealed that employing complex examination and treatment in women with infertility and intrauterine pathology is a prerequisite for subsequent ART protocols. IHC is a mandatory stage in the examination of women with endometrial pathology because of its reliability and accessibility for endometrial state assessment.
About the authors
Viktorija N. Abramova
St Petersburg State Pediatric Medical University
Author for correspondence.
Email: grantabramov@mail.ru
gynecologist, Gynecology Department
Russian FederationSergej N. Gajdukov
St Petersburg State Pediatric Medical University
Email: gaiducovsn@rambler.ru
MD, PhD, Dr Med Sci, Professor, Department of Obstetrics and Gynecology
Russian FederationAnna N. Tajc
St Petersburg State Pediatric Medical University
Email: annataits1@rambler.ru
MD, PhD, Assistant Professor, Department of Obstetrics and Gynecology
Russian FederationReferences
- Башмакова Н.В., Мелкозерова О.А., Винокурова Е.А., Пепеляева Н.А. Состояние здоровья новорожденных, рожденных от матерей с угрозой прерывания беременности // Проблемы репродуктологии. – 2004. – Т. 6. – № 2. – С. 28–29. [Bashmakova NV, Melkozerova OA, Vinokurova EA, Pepeljaeva NA. The State of health of the infants born to mothers with threatened abortion. Problemy reproduktologii. 2004;6(2):28-29. (In Russ.)]
- Гайдуков С.Н., Резник В.А., Антоненко В.С. Характеристика соматизированных расстройств пациенток с гиперпластическими процессами эндометрия в позднем репродуктивном возрасте // Педиатр. – 2011. – Т. 2. – № 4. – С. 82–84. [Gaydukov SN, Reznik VA, Antonenko VS. Kharakteristika somatizirovannykh rasstroystv patsientok s giperplasticheskimi protsessami endometriya v pozdnem reproduktivnom vozraste. Pediatr. 2011;2(4):82-84. (In Russ.)]
- Добротворцева О.А. Морфологические исследования эндометрия при различных формах бесплодия // Акушерство и гинекология. – 1987. – Т. 11. – № 12. – С. 25–29. [Dobrotvorceva OA. Morphological study of the endometrium with different forms of infertility. Akusherstvo i ginekologija. 1987;11(12):25-29. (In Russ.)]
- Ковалева Ю.В. Этиология хронического эндометрита. Хронический эндометрит. – СПб.: Изд-во Политехн. ун-та, 2010. – С. 73. [Kovaljova JuV. Etiology of chronic endometritis. Chronic endometritis. Saint Petersburg: Izd-vo Politehn. un-ta; 2010. P. 73. (In Russ.)]
- Колмык В.А., Насыров Р.А., Кутушева Г.Ф. Преимущества иммуногистохимического метода в диагностике хронического эндометрита // Педиатр. – 2015. – Т. 6. – № 1. – С. 11–15. [Kolmyk VA, Nasyrov RA, Kutusheva GF. Advantages of immunohistochemistry in the diagnosis of chronic endometritis. Pediatr. 2015;6(1):11-15. (In Russ.)]
- Корнеева И.Е. Современная концепция диагностики и лечения бесплодия в браке: Автореф. дис. … д-ра мед. наук. – М., 2003. [Korneeva IE. The modern concept of diagnosis and treatment of infertility. [dissertation] Moscow; 2003. (In Russ.)]
- Корнеева И.Е. Бесплодный брак. Современные подходы к диагностике и лечению. – М.: ГЭОТАР-Медиа, 2010. [Korneeva IE. Barren marriage. Modern approaches to diagnostics and treatment. Moscow: GJeOTAR-Media; 2010. (In Russ.)]
- Лаура Н.Б., Воронова О.В., Ковалева А.В., Хаджиева М.Х. Роль эндометрия в невынашивании беременности. Материалы IV Съезда акушеров-гинекологов России. – М., 2008. – С. 142. [Laura NB, Voronova OV, Kovaljova AV, Hadzhieva MH. The role of the endometrium in miscarriage. (Conference proceedings) Materialy IV S’ezda akusherov-ginekologov Rossii. Moscow; 2008. P. 142. (In Russ.)]
- Лунева И.С., Хуцишвили О.С., Иванова Т.С. Хронический эндометрит и привычное невынашивание беременности. Материалы XI Всероссийского научного форума «Мать и дитя». – М., 2010. – С. 128. [Luneva IS, Hucishvili OS, Ivanova TS. Chronic endometritis and habitual miscarriage pregnancy. (Conference proceedings) Materialy XI Vserossijskogo nauchnogo foruma “Mat’ i ditja”. Moscow; 2010. P. 128. (In Russ.)]
- Михнина Е.А., Давыдова Н.И., Комаров Е.К., Орлова О.О. Предгравидарная подготовка эндометрия у женщин с неспецифическим хроническим эндометритом и нарушением репродуктивной функции. Всероссийский конгресс «Амбулаторно-поликлиническая практика — новые горизонты»: сборник тезисов. – М., 2010. – С. 227–228. [Mihnina EA, Davydova NI, Komarov EK, Orlova OO. Predgravidarnaja preparation of the endometrium in women with nonspecific chronic jendometritom and violation of the reproductive function. (Conference proceedings) Vserossijskij kongress “Ambulatorno-poliklinicheskaja praktika – novye gorizonty”. Moscow; 2010. P. 227-228. (In Russ.)]
- Озерская И.А. Эхография в гинекологии. – М.: Медика, 2005. – С. 179–184. [Ozerskaja IA. Ultrasound in Gynecology. Moscow: Medika; 2005. P. 179-184. (In Russ.)]
- Побединский Н.М., Балтуцкая О.И., Омельяненко А.И. Стероидные рецепторы нормального эндометрия // Акушерство и гинекология. – 2000. – Т. 12. – № 3. – С. 56. [Pobedinskij NM, Baltuckaja OI, Omel´janenko AI. Steroid receptors of normal endometrium. Akusherstvo i ginekologija. 2000;3(12):56. (In Russ.)]
Supplementary files